Despite significant advances in the diagnostics and treatment of cardiovascular diseases, these diseases remain the leading cause of death across the globe. In most cases, they can be prevented according to Corresponding Member of the Russian Academy of Sciences (RAS), Deputy Head for Research Affairs at the Medical Research and Educational Center of Lomonosov Moscow State University (MSU) Simon Teymurazovich Matskeplishvili. In his interview with Scientific Russia, the cardiologist speaks about the prevention of these diseases and a new MSU and foreign scientists’ joint development, that is, a unique artificial valve for closed-chest heart valve replacement.
─ What is the role of heredity as opposed to that of lifestyle in the development of cardiovascular diseases?
― Cardiovascular diseases can be hereditary when parents pass defective genes down to their children. They can be either independent diseases, such as cardiomyopathy or heart rhythm disturbances, or part of complex hereditary diseases: Marfan syndrome and Ehlers-Danlos syndrome, to name but a few. There is a separate group of congenital heart defects that can develop due to genetic causes, but more often they result from fetal growth disturbances. Their cause is specific negative factors and external influences on fetal development during pregnancy, mainly in the first trimester. They are, for example, specific viral diseases (primarily rubella), mother’s bad habits, use of specific drugs, and exposure to ionizing radiation. Father’s health might be another important factor involved in the development of congenital heart defects. Factors that contribute to the risks of giving birth to a child with congenital heart disease are the mother’s age, spouses’ endocrine diseases, morning sickness, threatened miscarriage, and so on.
However, in most cases, the cause of cardiovascular diseases is a combination of genes and unhealthy lifestyle. The contribution of inborn risks here is not more than 20%, whereas the remaining 80% relate to acquired risks such as high blood pressure, smoking, unhealthy diet, overweight and obesity, alcohol abuse, and low physical activity. Almost all of them can be effectively managed, so most circulatory diseases can be considered preventable.
─ The same proportion of the contribution of inborn and acquired risks is relevant to oncological diseases.
― Exactly! As for the significance of external factors, for example, stress, I can provide an interesting example from my practice. When I was a student of the Department of Psychiatry at the famous clinic named after Sergei Korsakov at Moscow Medical Academy (now it is Sechenov First Moscow State Medical University), I treated a patient with epilepsy. She was a 50-year-old woman with severe and frequent epileptic seizures and pronounced pathological changes in the electroencephalogram. This woman had a twin sister with the same encephalographic abnormalities, but the latter had not had a single epileptic seizure in her entire life! What had triggered epilepsy in my patient? When I interviewed her, I found out that she had experienced a serious psychological trauma at the age of six: they were celebrating New Year, she was dressed as a Snow Maiden, they were burning Bengal fire sticks, and her dress would catch fire. She got burned and this was a huge stress, of course. Her genetic predisposition manifested itself as clinical epilepsy afterward. Again, her sister had absolutely the same genes and the same abnormal encephalogram. In my opinion, although this example is from a different field of medicine, it clearly illustrates that heredity does not always determine disease development. It is especially relevant to circulatory system diseases. Certain genetic factors related to cholesterol metabolism, coagulation, thrombosis, structure, and functioning of blood vessel walls can be significantly enhanced or weakened by people’s lifestyle, diet, presence or absence of physical activity, their reaction to stress, and so on.
─ To what extent are stress and cardiovascular diseases interrelated?
― Stress exposure correlates with the probability of developing major cardiovascular diseases. The World Health Organization (WHO) reports that the main cause of death on Earth is diseases associated with high blood pressure, that is, not arterial hypertension as such but any condition leading to it: myocardial infarction, stroke, heart failure, and others. In most cases, arterial hypertension is a consequence of stress, usually a chronic one. Yes, a small share of hypertension cases, 5-10% at best, is caused by other diseases, that is, polycystic kidney disease or renal artery stenosis, thyroid dysfunction, and adrenal disorders. All the rest though is a direct consequence of chronic stress. Chronic stress leads to coronary heart disease and cerebral accidents, namely, strokes, as well as diabetes mellitus, various gastrointestinal diseases, and so on. Stress is considered to be one of the core risk factors along with smoking, high cholesterol, high blood glucose levels, and overweight. Therefore, when we examine patients, we have to assess their level of stress and reduce it.
─ What is your opinion about the idea that the high prevalence of cardiovascular diseases is among all else associated with the unbalanced omega-6/omega-3 ratio that results from high consumption of meat and low consumption of fish? After all, it is well known that, for example, Eskimos have a lower prevalence of cardiovascular diseases than Europeans.
― Yes, it is true. It is well known that the residents of countries with high consumption of fish and seafood are at relatively low risk of developing cardiovascular diseases. It applies not only to Eskimos or the Japanese but also to those who follow the Mediterranean diet where fish is not the only source of polyunsaturated fatty acids. This diet is popular in Italy, Portugal, France, and other Mediterranean countries.
In addition, according to the recently published research findings, adding omega-3 polyunsaturated fatty acids to statin therapy in patients at a very high risk of cardiovascular complications with high triglycerides resulted in a 26% reduction in mortality due to myocardial infarction and stroke. These findings provided grounds for approving the use of this food supplement that contains eicosapentaenoic acid, essential fatty acid and the main component of omega-3 polyunsaturated fatty acids in fish and shellfish, as a medicine to improve treatment outcomes in patients with coronary heart disease and hypertriglyceridemia.
Let’s get back to the Japanese and Eskimos. It is also important to remember that, in addition to eating a lot of fish, they live in certain environmental conditions that are habitual to their body from early childhood. Interestingly, the risks of developing severe cardiovascular diseases are much higher for the Japanese who move to Europe or the United States. Therefore, healthy products alone are not enough. In my opinion, it is also important to live in a geographical area where these products are part of the lifestyle.
─ If a person who has been eating meat throughout their life switches to fish, will the risk of cardiovascular diseases decrease?
― I believe it is possible. However, it is not enough to just switch from meat to fish: if you eat fish with a large slice of bread with a great deal of butter scraped over it, then nothing will change on a global scale. Fish is just part of your diet and lifestyle which may need to be revised largely if we want to achieve long-lasting healthy changes.
We know quite many cases of longevity and low cardiovascular mortality in regions that are quite far from seas or large rivers and where people’s diet consists of animal meat or poultry. Today, many people continue eating meat but change other eating habits, that is, stop eating processed food and significantly reduce the intake of salt and products with trans fats. It allows them to substantially improve their health and dramatically reduce the probability of developing cardiovascular diseases.
Simon Matskeplishvili, RAS Corresponding Member, scientist, cardiologist of high category, winner of the Russian Federation Government Award for 2012
Photo: Elena Librick / Scientific Russia
─ Many factors influence the development of cardiovascular diseases. Can you name one core factor?
― I can, but first things first. There are several key risk factors that everyone is aware of. These are high blood pressure, smoking, high cholesterol, and high blood sugar. However, if you ask me, I would say stress is the core factor. It is the modern scourge. The second most important factor is low physical activity. These factors are interconnected. Severe stress and anxiety are the main reasons for the development of arterial hypertension, tobacco addiction, and obesity with accompanying high cholesterol, blood sugar, and so on. Of course, high blood pressure can be caused by other diseases, you can start smoking at school, and diabetes can be hereditary, but most often these conditions are the consequence of serious psycho-emotional distress. You may ask: how to manage it? The best way is regular physical activity. It is very important as no or low physical activity is the top risk factor for multiple diseases, not only cardiovascular diseases but also oncologic, metabolic, and musculoskeletal disorders, to name but a few. I hope that our development of physical culture and sports state program will encourage people to engage in physical activity, such as walking or cycling, more often which will help to change the situation largely.
We know well how to manage high blood pressure, high sugar, and high cholesterol. However, we have not succeeded in engaging people in physical exercises and sports yet. The more active people are, the longer their life is.
─ Is the global burden of cardiovascular diseases still the biggest one, is it bigger than that of oncological diseases? Can we explain it by the fact that, as they say, people die before they develop cancer?
― It is a very interesting question. Circulatory diseases remain the main cause of death on our planet, far ahead of oncological or infectious diseases, respiratory diseases, gastrointestinal disorders, or diabetes mellitus. At the same time, they are getting younger, and more and more patients die at a relatively young age. As for oncological diseases, there is also a direct relationship between age and the risk of developing cancer in both women and men: the older the person, the higher the risk. Therefore, if a patient dies of a heart attack, stroke, or heart failure at a relatively young age, it is likely they died before they could actually develop cancer. On the other hand, it is important to understand that, as opposed to malignant neoplasms, most cardiovascular diseases can be prevented. If we could effectively promote healthy lifestyles at a large scale, implement regular health examination, ensure a comprehensive control of risk factors in our lives, we would achieve a significant decline in cardiovascular mortality all over the world.
Now, however, there is circulatory disease supermortality in Russia. Even if we consider statistically adjusted data, our mortality rates are dozen times higher than those in western countries. This is a good reason to finally revise our approach to the treatment and prevention of cardiovascular diseases.
─ Scientists from MSU and their foreign colleagues have recently developed a unique artificial valve for closed-chest heart valve replacement. Please tell us about this unique technology.
― This technology has not been used anywhere in the world before. It is a great honor for me to be a member of a wonderful team at the University of Cape Town (UCT), South Africa that implemented this international project. Austria, Germany, China, and the USA also took part in this project. Some research studies took place at Groote Schuur Hospital. In December 1967, Christiaan Barnard performed the world's first successful heart replacement at this hospital. The project is led by Professor Peter Zilla, a world-famous cardiac surgeon who heads Christiaan Barnard Center at UCT.
You can say that we already have valves that can be implanted in the heart without opening the chest (using the so-called transcatheter technologies) through a small incision in the heart or femoral artery. However, even these advanced technologies have significant drawbacks that we managed to overcome when developing our unique technology.
Almost all the components have no analogs in the world, that is, the frame that was designed based on mathematical analysis and modeling of the anatomy and hydrodynamics of the aortic root; artificial leaflets made of an innovative polymeric material; valve delivery system and opening balloon of a unique helical form; the use of 3D printing in production, and more.
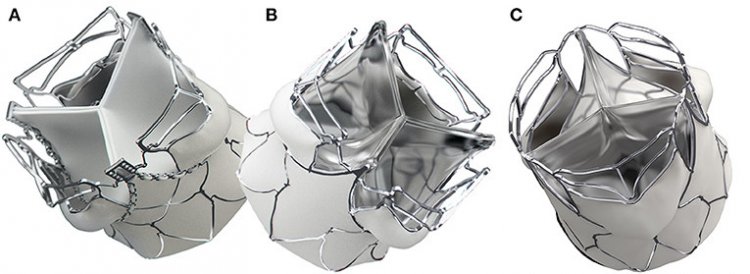
SAT balloon-expandable transcatheter aortic valve replacement (TAVR) valve. The direct bonding to the MP35N-scallop (MP35N is a nickel-cobalt alloy with unique increased durability, flexibility, resilience, corrosion resistance, and biocompatibility parameters – editor’s note) allows for an optimal attachment of polymer leaflets to the metal stent. Both the supra-annular anchorage arms and the spacer arms are structures that are self-installed due to plastic deformation. The first generation SAT TAVRs show minor differences between the bioprosthetic (A) and the polymer version (B). The second-generation “universal” stent (C) supports both bioprosthetic and polymer leaflets and allows crimp-diameters for trans-femoral (through the femoral artery – editor’s note) access. Source: Frontiers Media.
The new shape of the valve frame and anchoring mechanism of the artificial valve allow implanting this device not only in elderly patients with calcified aortic stenosis but also in young people with aortic valve insufficiency and patients with rheumatic aortic valve disease. This group comprises a huge number of people who have to undergo a long and complicated open-heart surgery at the moment.
The polymer, which uses a completely new type of polyurethane, is protected against a very aggressive environment in our body. It is practically eternal as opposed to the biomaterials of currently available artificial valves. They serve for ten or, at best, fifteen years. The valve delivery system and installation process are so simple that this procedure can be performed in regular surgical settings. It does not require a very sophisticated, extremely expensive, and rarely available cardiosurgical operating unit. It significantly improves the availability of this type of medical care, including for developing countries, as well as for the Russian regions that do not have a well-developed cardiovascular surgery service now.
Our development has many other unique features. The most important thing is that we have managed to significantly expand the pool of patients who can benefit from this technology. We have introduced a simple, effective, available, and, importantly, inexpensive technology that can save the lives and health of millions of people. In my opinion, if we develop and actively use this technology in clinical practice, and we are completely ready for this, it will revolutionize the treatment of heart valve diseases.
We have another technology under development for the treatment of severe mitral valve regurgitation. It is a very serious problem. This development also promises to be revolutionary.
I believe that one of the top-priority tasks that we, as a teaching clinic of the leading Russian university, should solve is the active implementation of diagnostics and treatment of patients with heart valve diseases. This problem is extremely acute in our country, and it has not been solved so far. I will give you an example. A large number of young women with mitral valve prolapse do not have children, as they are afraid (most commonly unreasonably) of complications during pregnancy and childbirth. Equally many elderly patients with severe aortic valve stenosis and other serious diseases refuse to undergo treatment, as they fear complications. This problem must be solved as quickly as possible. We plan to develop and widely introduce an educational program on valvular heart diseases to help a very large number of people.
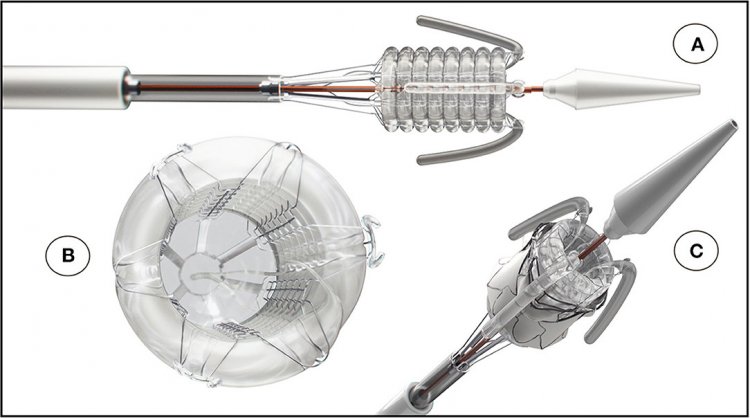
The SAT non-occlusive balloon-delivery system consists of a helical balloon and is prevented from toppling by a Nitinol frame; (A, C) positioning- and stabilizer-trunks that are invaginating upon retraction; (B) a back-flow valve and a pressurized rolling sleeve for device retrieval. Source: Frontiers Media
─ Please tell us a bit more about the main components of your new technology, that is, the equipment for closed-chest heart valve replacement.
― I've already told you about the revolutionary balloon that has a helical form to avoid complete occlusion of the left ventricular outflow tract lumen during deployment. It saves doctors and patients from serious problems. I will try to explain, but I should first say a few words about the approach that is now used in the world. Imagine a beating heart. Each contraction ejects blood into the aorta, the main artery of our body, under high pressure. The aortic valve is located in the place where the aorta originates from the left ventricle of the heart. We have to place our valve in this place, just like a stent is placed in the coronary artery. Since an artificial valve is delivered to the implantation site through a special tube called a catheter, it is initially strongly compressed using a special device so that it is more compact and fits in the lumen of the catheter. There are two artificial valve installation technologies: it either opens due to shape-memory materials or uses a special balloon, again, just like a vascular stent. However, even self-expanding valves require a balloon either for pre-dilatation (preliminary widening of the implantation site) or additional expansion of the valve after its installation. Even short-term inflation of such a balloon in a beating heart, which is, in fact, a complete blockage of the blood flow from the heart to the aorta, can lead to serious consequences, especially in case of severe myocardial damage that often accompanies aortic valve defects: acute hemodynamic depression, severe arrhythmia, cerebral hypoxia or even death.
To avoid this situation, the technology of artificial ultra-frequency electrical stimulation of the left ventricle is used. It ensures a heart rate of 150-180 beats per minute, which practically means a temporary mechanical cardiac arrest. The time of this stimulation should thus be minimized, so manipulations with the artificial valve and balloon must be very quick. Therefore, sometimes not one but several episodes of ultra-frequency stimulation are required. This technology is relatively safe when used by an experienced professional, but there are few of them.
Our balloon has a helical form and a wide internal lumen, which makes it possible to completely abandon this stimulation technology and have an almost unlimited period of time to perform precise manipulations in a calm atmosphere and place the valve in the required position. In addition, our balloon can be used with any existing type of artificial valve, which allows increasing the safety of this procedure significantly and makes the procedure available to a larger number of patients with severe heart diseases.
A very important achievement is the development of new polymeric material based on polyurethane that is protected against the aggressive internal environment of our body or immune system. From the viewpoint of its mechanical properties, it is many times superior to all existing artificial valves. 250 million valve opening and closing cycles are required for new artificial material to get approval. Our valve remains almost intact even after one billion cycles. There is no cracking on the surface or fringing at the edges of the leaflets. It will allow extending the age limits and including younger patients who normally receive mechanical heart valves at the moment. These valves require lifelong therapy with blood thinners and blood clotting control at least once a month. Again, we hope that we will soon manage to provide evidence of the effectiveness of our technology and introduce it into clinical practice.
― Simon, please tell our readers what they can do to protect themselves from cardiovascular diseases. What medical tests should they undergo and what lifestyle should they have?
― It is possible to completely defeat cardiovascular diseases, but it is not easy. No country has managed to do that yet, although some states have made significant progress in this area. However, it is important to understand that circulatory diseases are, in most cases, preventable, and it is prevention that we should focus on to improve the situation with circulatory diseases in our country and, consequently, prevent a significant number of sudden cardiac deaths.
─ How do we do that?
― By minimizing the risk factors that we have already discussed today: smoking, overweight, insufficient physical activity, consumption of salt, sugar, fast-digesting carbs, and sleep deprivation. Today we are witnessing a real pandemic of diabetes mellitus and cardiovascular diseases that it causes. Another important factor is stress which has evolved into a huge problem all over the world.
Talking about the medical aspect of this problem, then, as you know, periodic health examination is very effective. Men and women who have reached the age of 40-45 years should see a cardiologist once a year and undergo a series of simple tests – clinical and biochemical blood tests, lipid profile, and, if necessary, glycated hemoglobin. It is very important to perform coagulation tests to measure coagulation. Of course, it is important to measure blood pressure and do that on both arms.
Another simple test that I recommend is the exercise test. This fairly simple diagnostic helps to identify patients with low risks of developing cardiovascular diseases or their complications. If an adequately performed stress test in a patient is negative, then this person is unlikely to suffer a myocardial infarction or some other serious complications within the next year.
WHO: Cardiovascular diseases (CVDs) are the leading cause of death globally, taking an estimated 17.9 million lives each year. CVDs are a group of disorders of the heart and blood vessels and include coronary heart disease, cerebrovascular disease, rheumatic heart disease, and other conditions. More than four out of five CVD deaths are due to heart attacks and strokes, and one-third of these deaths occur prematurely in people under 70 years of age.
Photo: hywards / 123RF
Of course, there are much more elaborate and complex tests: cardiac calcium scoring and coronary computed tomography angiography (CCTA), cardiac magnetic resonance imaging (MRI), or even a heart positron emission tomography (PET) scan. Or, there is invasive coronary angiography, which I do not approve of by the way.
All these methods have been known for a long time, but some of them are not popular in our country. However, the main diagnostic and even treatment method in cardiology is communication between the doctor and the patient, mutual trust and agreement on examination and treatment tactics. But there is no time for this left in modern medicine. However, we cannot provide care to patients without a thorough and detailed explanation of the importance of lifestyle changes, compliance with recommendations, the need for long-term, sometimes lifelong, intake of specific medicines, serious diagnostic or therapeutic procedures, or even heart surgeries.
To improve service provision in the primary health care, MSU has developed a special system that helps to collect information on a patient’s physical condition: it obtains and analyzes the main physiological indicators and vital signs in just 7–10 minutes using our software and hardware. This research field is, indeed, important, it is supervised by the head of our medical center, academician Armais Kamalov. By using our risk assessment algorithms, we can identify moderate- and high-risk patients who need to be further examined in more detail and probably treated. I think that if such programs are implemented into our healthcare system more widely, the results must be positive. At the moment, unfortunately, mortality from circulatory diseases remains unacceptably high, and COVID-19 has also contributed to this. We have something to work on and something to strive for, and sooner or later we will defeat cardiovascular diseases, I am sure of that, but to do so we must work very hard and rigorously.