The Institute for Nuclear Research (INR) of the Russian Academy of Sciences (RAS) has developed a method for the instantaneous destruction of cancer cells: now this so-called ultra-flash therapy is being tested using tumor cell cultures. The new approach was created thanks to the largest Eurasian linear proton accelerator operating in the institute.
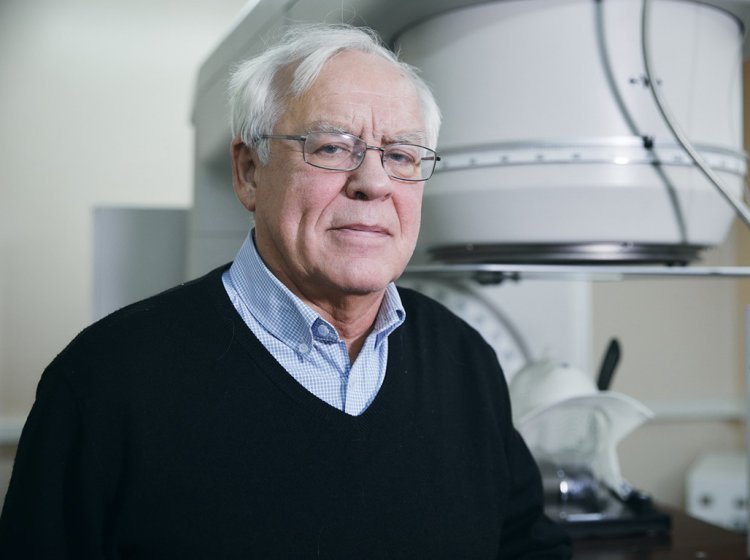
Doctor of Physical and Mathematical Sciences and Head of the Medical Physics Laboratory at INR RAS (Troitsk) Sergey Vsevolodovich Akulinichev has shared the details of this research with a Scientific Russia correspondent.
― Is it true that your accelerator is the only device in the world that makes it possible to deliver a radiation dose to a tumor in such a short period of time?
― There are so-called single-pulse proton accelerators in the world, but our device actually stands out from them, as it allows us to deliver the entire therapeutic dose of a medicine to a tumor in just one shortest possible pulse. I do not know such examples in the world. The INR RAS accelerator has made it possible to deliver the entire radiation dose to the tumor target in 100 μs (0.0001 s) for the first time ever.
― Do you conduct your research on cultured cancer cells rather than humans at the moment?
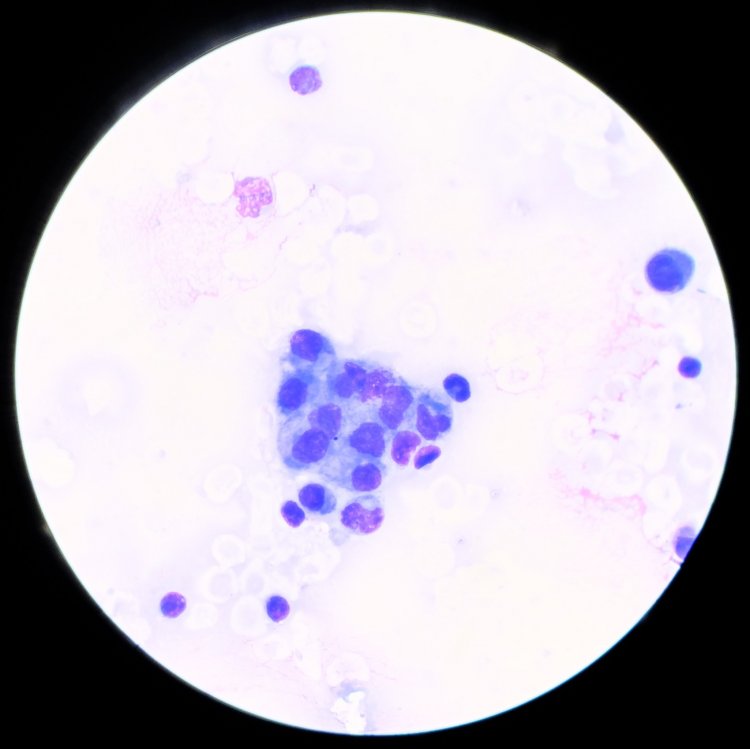
― Yes, you are right. We are at the beginning of a long journey. In our experiments, we irradiate tumor cells and normal cells in laboratory plasticware and compare their responses to the doses delivered in different modes, including the single-pulse mode. No one has ever been treated using the ultra-flash mode, and it is healthcare professionals who will have to assess the justifiability and safety of this treatment in the future. As for us, we have already managed to achieve the complete destruction of tumor cells at the cellular level through apoptosis by irradiating them with a single pulse, while normal cells are not damaged in this mode with the same dose. This is our key result for today.
― What is the fundamental difference between this method and the conventional proton beam therapy?
― The difference is that, in our case, we use single dose delivery, that is, with one fraction of ionizing radiation delivery, while the conventional proton beam therapy usually requires about 20 fractions. Flash therapy is being actively developed in the world, and this therapy helps deliver the dose in a fraction of a second: in half a second or less. However, it is inferior to ultra-flash therapy in exposure intensity and rate, since we irradiate the target in a fraction of a millisecond using the ultra mode.
Proton therapy helps deliver the radiation dose exactly to the tumor: not only by the coordinates transverse to the beam but also by the depth. Protons literally stop in the tumor at a given depth. Other types of radiation often pass through the patient irradiating everything in their path. Photo source: mackoflower / 123RF
― I have heard that you managed to affect even a radioresistant tumor.
― Yes, we conducted such experiments. We irradiated and examined three types of cells: tumor radioresistant, radiosensitive, and common cells. The ultra-flash mode does significantly more damage to radioresistant cancer cells as opposed to that of the conventional flash therapy. The study covered only apoptosis – it is an important but hardly the only way of cell death. There are also necrosis, membrane destruction, and other types of cell death. In the future, we will have to analyze the complex response of cells to this irradiation mode, including studying the response of genes to this intervention. Having received a comprehensive analysis of the cellular response to ultra-flash irradiation, we will be able to claim that we have proved a therapeutic effect at the cellular level. Experiments with animals will take place after that.
― Why do cancer cells react so strongly to this type of irradiation? What is the mechanism behind this response?
― There is still no answer to this question. Many biologists tried studying this mechanism. This subject has become especially relevant in the past few years. In late 2022, a major international conference in Spain was devoted to the discovery of flash effect mechanisms. Now we are analyzing the materials from this conference.
At the moment, we see the following: the flash effect actually works, but the biological foundation of this effect on cells has not been finally formulated.
― Why dis ultra-flash therapy begin to develop based on the INR RAS accelerator only in the past few years? After all, this accelerator has been in operation since the 1980s.
― Indeed, it was impossible to immediately associate the extremely high intensity of our accelerator with a possibility of instantaneous tumor destruction. Earlier we believed that too high radiation intensity is useless for the radiologist while only complicating the treatment. Besides, such a high dose rate requires new dose monitoring methods, since the standard dosimetry methods using ionization chambers do not work very well in this case. That is why we are currently developing some new equipment for ultra-flash therapy and have already tested a new detector developed at INR RAS. New treatment options require new detection methods, so we still have a lot of work to do.
The INR RAS accelerator makes it possible to deliver the entire irradiation dose of 40–50 Gy in 100 μs, which is 5,000 times faster vs. the conventional flash mode. This ultra-short irradiation does five to six times less damage to normal cells through apoptosis vs. the conventional radiation therapy. Photo source: Elena Librik / Scientific Russia
― We are at the INR RAS Proton Therapy Center. It would seem reasonable to see some patients here, but there are no patients at the moment. Why so? Do you plan to work not only with cultured cells but also with living people in the near future?
― In fact, none of our radiation units is used to treat patients at the moment. Speaking specifically about the proton beam unit, we have not mastered the technology well enough to treat patients. We are currently working only with cellular material and, as I have said above, after that we are going to conduct trials on animals. A permit for clinical trials on volunteers can be obtained only after the safety and efficacy of ultra-flash therapy are proven in animals.
Proton therapy helps deliver the radiation dose exactly to the tumor: not only by the coordinates transverse to the beam but also by the depth. Protons literally stop in the tumor at a given depth. Other types of radiation often pass through the patient irradiating everything in their path. Photo source: toeytoey / 123RF
― How long can this procedure take?
― This period is measured in years, and the procedure requires special funding: accelerator sessions are very expensive and energy-consuming. In my opinion, we need at least three years and, probably, even more to switch to clinical trials with volunteers. We cannot skip certain stages of preclinical and clinical studies and have to pass all of them with good results.
― Apparently, there are many people who would want to receive this treatment. Can volunteers sign up for the upcoming clinical trials right now?
― We do not make any decisions about the people who get to us for experimental treatment. These decisions are made by the attending doctors of particular patients. Proton beam therapy, including ultra-flash therapy, is used in several facilities across our country. They are usually hospitals where the patients are registered or scientific medical institutes to issue referrals for such treatment. Only doctors can decide what treatment method is suitable for a particular patient, and they are also responsible for making sure the prescribed treatment is correct. Therefore, as you can see, patients cannot sign up for ultra-flash therapy on their own. Besides, a proton beam unit has to be licensed and authorized for clinical trials with volunteers. This practice has been developed over years and, in my opinion, it absolutely justifies itself.