COVID-19 is becoming more insidious and dangerous. Thus, the new delta strain of the coronavirus is recognized as dominant throughout the world, while the disease course is much more severe. At the same time, people often feel quite well during the first days of their illness. They sometimes experience only mild fever, barely noticeable cough and runny nose. However, they simultaneously develop hypoxemia and are later hospitalized with serious lung damage
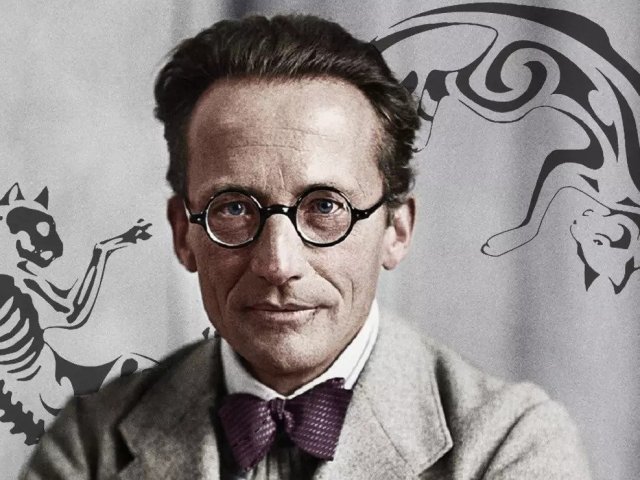
Sergey Nikolaevich Avdeev – Director of the Clinic of Pulmonology and Respiratory Medicine at I.M. Sechenov First Moscow State Medical University, Head of the Pulmonology Department, Chief Consulting Pulmonologist of the Russian Ministry of Health, Corresponding Member of the Russian Academy of Sciences.
− Sergey Nikolaevich, the incidence of COVID-19 and mortality caused by it soared again in November 2021 in Russia. What are the reasons, in your opinion?
− Several factors are important here. First, there has emerged a new strain – the more aggressive, more virulent delta strain. Second, Russia still has a low level of population vaccination.
Unfortunately, our country takes one of the last places in the world level of vaccination. This is a true fact. Russia is not even included in the first hundred.
There is only one solution here – to undergo vaccination. Every person should do that. We will be unable to cope with COVID-19 without it.
− Doctors often say so, but many citizens do not trust the vaccines anyway.
− Unfortunately, doctors’ opinion gets lost against the background of the opinion shared by so-called “anti-vaxxers.” It is also surprising that Russia has an unprecedentedly high level of anti-vaccination campaigns. Our country takes the first lines in this rating too. There is no similar situation anywhere in the world. This is real obscurantism. I cannot say anything else. At the same time, it is impossible to find logical explanations.
− Has the new strain brought new distinctive peculiarities of the course of this disease that have not been observed before?
− Yes, of course. Today this information is coming from everywhere. The disease course follows a faster and more dangerous scenario. Besides, the incubation period has decreased, while severe disease forms have become more common in young people and people without concomitant diseases. Red zones see children more and more often. Therefore, of course, we notice a difference in comparison with the situation that took place one year ago, and this difference is serious.
High-resolution computed tomography (lung lesions in the form of “ground glass,” 100%)
− What effect does COVID-19 have on patients’ lungs?
− Coronavirus patients have more serious lung damage determined by a number of anatomical terms. We see damage, inflammation and blood clotting. Unfortunately, the lungs are the most vulnerable and heavily affected system in case of COVID-19.
The lungs are a gateway for this infection. The coronavirus infection is an airborne disease. Consequently, the infection enters the body through the respiratory tract and epithelium, through cells called alveolocytes.
− Why does our immune system turn against us in case of this disease?
− We do not fully understand why it happens. However, our immune system cannot be considered ideal either. At some moment, the immune system starts fighting the infection so vigorously that it affects our own tissues and organs.
− Is it known why the lungs do not send signals about the danger at all, while lung damage is detected either at more advanced stages when shortness of breath develops or on X-ray scans?
− It is not really true. Usually, the body sends such signals in the form of coughing. However, talking about shortness of breath, indeed we see specific paradoxes in case of COVID-19, including the so-called phenomenon of silent hypoxemia. In this case, patients may have hypoxia or oxygen starvation, but they experience no shortness of breath. Unfortunately, the symptoms do not always develop in parallel.
Besides, some patients develop asymptomatic pneumonia when severe lung damage is detected through image diagnostics, but patients do not feel anything.
We should remember that each person can have an individual response to this disease. For example, some patients have 5% lung damage and they immediately feel unwell. However, others feel nothing until their lung damage becomes 50% at which point the body usually sends signals about changes being sometimes catastrophic. Why does it happen? There is no unambiguous answer at the moment.
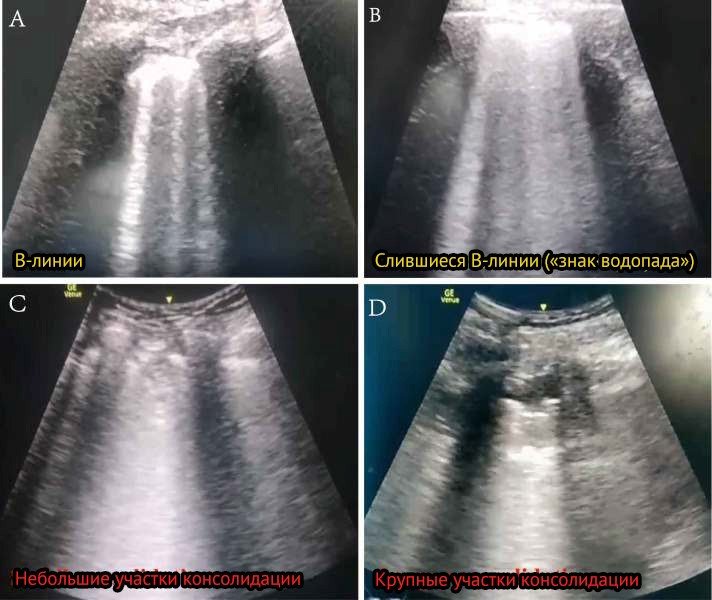
Ultrasound lung examination in case of COVID-19
− What do doctors do in this situation? How do they treat such lung damages?
− Diagnostics is of prime importance here and we cannot manage without a simple pulse oximeter in this case. I believe there are no people being unaware of this device now. This small, portable tool is extremely useful. It gives us important information on several parameters, but the most significant one is saturation, that is, the value of blood oxygen saturation. This biomarker reflects the development of hypoxemia or respiratory failure.
However, of course, we use more methods. Doctors turn to an entire range of laboratory, instrumental methods, image diagnostics. This is the only way to make up a “mosaic” of different elements to better understand what is happening to our patient.
− What are the current approaches to recovering the affected lungs?
− The first thing we start with is antiviral therapy. However, it is not always possible to use it for this or that patient. For example, if we hospitalize patients in five-six days after the disease onset, using antiviral therapy is senseless.
Next, doctors fight the syndromes caused by this disease. Here we use anti-inflammatory therapy, therapy meant to eliminate coagulation disorders and, finally, therapy to defeat hypoxemia or respiratory failure.
Of course, each patient may have their own, unique peculiarities of the course of this disease, so their therapy will be different in each case.
− Have new diagnostic methods and treatment approaches appeared?
− Talking about diagnostics, for example, pulse oximetry is now introduced into all levels of medicine. Only pulmonologists used to take pulse oximeters along earlier, but today every doctor of any specialty has it at hand. People buy this device and use it at home too.
However, there are methods that were given a development impetus right by the pandemic. For example, ultrasound examination of the lungs. This technique was known and actively used before it too, but it has become widespread right now. And I hope that this method will stay in our practice even after we fight COVID-19.
However, there are specific areas of disappointment as well. As you might remember, the first list of antiviral medicines was very extensive. We were using medicines applied in rheumatology, in the treatment of HIV infection and neurological diseases. However, today the list of antiviral medicines is very short. At the same time, new medicines, including those based on monoclonal antibodies, will appear very soon and will be included in the list of medicines used to treat COVID-19.
The situation is changing fast. Two years have passed, but we do not stop our search and are constantly looking for new medicines and more effective treatment methods.
− What can help patients rehabilitate after this disease?
− There is no single scenario here. Everything strongly depends on what problems patients face after their illness. The well-known post-COVID syndrome includes a number of associated problems. This is kind of a “tangle” accompanying people who, at first glance, have coped with this disease.
For example, the most common ones are fatigue, shortness of breath, depression, insomnia, coughing, etc.
As for severe lung damage, in this case we do largely the same as when we manage pulmonary fibrosis. Usually, the damage is accompanied by the appearance of scars that are almost impossible to get rid of. These changes cause shortness of breath, coughing, people do not have enough breathing for physical work.
Conversely, some patients may develop cavitary lesions in their lungs. In fact, they are areas where lung tissue is missing. Such disorders are very dangerous and may cause pneumothorax, that is, accumulation of air or gases in the pleural cavity, bleeding and infection.
− What issues were acute before COVID-19?
− Actually, we had and still have a lot of problems. Asthma, chronic obstructive pulmonary disease (COPD), pneumonia. For example, pneumonia is similar to the coronavirus infection. In both cases, we see lung damage, disorders leading to respiratory failure. However, the treatment methods are completely different. Common pneumonia is treated with antibiotics that are ineffective for COVID-19.
− Talking about the educational component, how serious is the problem of staff shortage?
− Staff shortage really exists. There are not that many pulmonologists in our country in comparison with other medical specialties. This is understandable, as most pulmonologists are today working in the red zone. It means that there are not enough specialists to treat other diseases, such as asthma, pulmonary fibrosis, etc.
− Do you cooperate with your colleagues from other countries?
− Yes, we do. We have been exchanging experience with our foreign colleagues almost since the very start of the pandemic. It would be impossible to solve the tasks facing us without that. When we first faced the new coronavirus infection, we had no experience. However, we were borrowing it from our Chinese and then our European colleagues. This exchange continues today. We see each other at conferences and international forums where we discuss the main treatment aspects and methods.
− What can you say about the current situation in red zones?
− I said in the very beginning of our discussion that today there is a new outbreak of disease incidence. It means that the burden on doctors has again increased. However, I mean not only those who work in the very red zones. I am also talking about doctors at polyclinics, specialists working at ambulance stations, nurses and hospital attendants. I mean everyone employed in the healthcare system.
− The only solution is vaccination, isn’t it?
− Yes, it is. We should not hope that everyone will experience this disease and the pandemic will be over. After all, this path is associated with numerous losses, including among healthcare professionals.
The interview was conducted with the support of the Ministry of Science and Higher Education of the Russian Federation and the Russian Academy of Sciences.