When will the pandemic end? Will the Omicron variant, discovered in November, replace the dominant Delta? Can the epidemic end if people stop getting vaccinated and taking precautions?
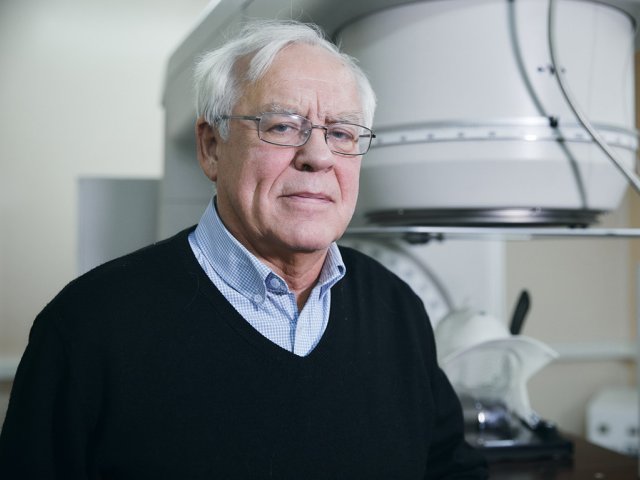
Scientific Russia discussed these issues with Anatoly Davidovich Altstein: Doctor of Medical Sciences, Professor, Chief Researcher of The Gamaleya Center.
– Are virologists making predictions about the end of the pandemic? When can the disease disappear?
– Any accurate forecasts can now be given only with a high degree of doubt. Now humanity has several quite effective vaccines: mRNA vaccines, adenoviral vector vaccines, whole virion inactivated vaccines. And new developments are on the way. Although I don’t know if they will play any role already. But the vaccines that are being used now are quite effective. This fully applies to the Russian Sputnik V vaccine and its variants.
A good result is also shown by various anti-epidemic measures that have been widely disseminated. This includes wearing masks, distancing people, and washing hands – all this is the right anti-epidemic behavior, which, unfortunately, is not observed everywhere.
I tend to think that if we use everything that modern science and medicine have achieved and adhere to anti-epidemic rules, then the epidemic will end, or mostly end, already in 2022.
– Now many scientists and health care organizers note that an insufficient part of humanity has been vaccinated. Can the pandemic end with an insufficient number of vaccinated people?
– Yes, the pandemic will end one day in such a situation too. But it is unclear how many years it will take, and how many victims will be in the end. It is very difficult to predict such a situation, but now everything is in our hands – as humanity wants, so the situation will develop. If we follow the recommendations, especially on vaccination, the epidemic will go away much earlier.
– Now the incidence in Russia has declined, although in October and November up to 40 thousand new cases were registered daily. Was it the peak of the pandemic in Russia, or should we wait for new outbreaks?
– That was the peak of the Delta variant. At the current stage, Delta is the most severe and most stable variant of all that we have encountered.
The very first variant was the Wuhan one: it’s a highly lethal variant, but where is it now? Then the British variant appeared – and also disappeared. There were South African, Brazilian, and Peruvian variants: they have left their sad mark, but now only Delta dominates. And I think the same situation will arise with Delta as with the previous strains – it will disappear, but it’s hard to say how long it will take. If vaccines and anti-epidemic measures are employed, it will probably take no more than a year. If we ignore all the recommendations, it is difficult to predict the timing.
It is also important that one variant can be replaced by another, and then everything must start almost from the beginning – this is the situation that arose with the Delta variant. In many countries, a significant number of people were vaccinated in the first half of 2021, including those who are at-risk – people with chronic diseases and the elderly. The Delta variant appeared after mass vaccination and brought a new wave of morbidity. Of course, vaccinated people got sick less frequently and had milder symptoms, died less often, but the effectiveness of vaccines declined compared with the British variant.
– That is, 40,000 cases in Russia are the spread of the Delta variant?
– Yes, and this increase began in June. Then they said that the third wave was coming, but summer came, and the incidence went down. After all, coronavirus infection is more or less season-related. With the beginning of autumn, the number of cases began to grow again, and this is a continuation of the wave that began in June. The autumn increase in cases is called the fourth wave, although it can be considered as a continuation of the third. The essence of this will not change.
– Tell us in more detail about the link between coronavirus infection and seasonality. On statistical charts, most peaks occur during the cold season, although some cases of increased incidence are also visible in summer. How can we characterize the seasonality of the coronavirus?
– In summer, people are more dispersed. They do not gather indoors as much as in the cold season, and the incidence of all respiratory diseases decreases – this applies not only to the coronavirus. Their time is late autumn and winter.
The coronavirus pandemic is not strictly following this path. Due to the high contagiousness, the virus can manifest itself regardless of the season, although the maximum peaks of morbidity occur in autumn and winter. In September, the rise began, it continued in October and reached its peak in November.
– Now one of the hottest coronavirus topics is the new Omicron strain. How well has it been studied, what mutations does it carry, and do existing vaccines protect against it?
– This variant was discovered only in November. It is associated with diseases in South Africa, and so far, there are no reports that it causes a severe form of the disease with a fatal outcome – one such case has been reported in England. This does not mean that it cannot cause severe form at all, more information is needed. I think that the lethality of the Omicron variant will be lower than that of Delta. By the way, Delta does not cause a high mortality rate in most countries: about 1.8% – 2%.
32 mutations in the S-protein gene of the new variant and about 20 more mutations in other genes seem a good sign to me. This is a sign that the virus genome may be unstable. With the help of mutations, the virus adapts, can reproduce better, but the virus doesn’t need to cause severe forms of the disease and kill, and with numerous mutations, lethal properties can decrease.
– That is, the spread of the Omicron variant can help humanity in the fight against the pandemic?
– I do not rule out such a development. At the same time, I do not rule out that Omicron will not spread as steadily as the British variant or Delta. There are no clear signs, looking at which we can confidently say whether the new variant will displace the previous one or not. Omicron is highly contagious and multiplies rapidly.
Not so long ago, information appeared from an authoritative scientist Ichiro Inoue from Japan – he is a well-known specialist in genome research and the determination of nucleotide sequences. He followed the progress of epidemics in Japan. Now in a day, you can get information about the complete genome of the virus, this is already routine work. Ichiro Inoue found that the number of mutations in the Delta variant increases during the decline of the epidemic, which leads to the weakening of the virus, up to extinction.
We can recall the history of epidemics of the 20-21st centuries.
In 1918-1919 there was the Spanish flu that claimed the lives of millions. The pandemic ended (the mortality rate from influenza is now 0.1%, although the causative agent of the Spanish flu virus A H1N1 influenza has remained, and now behaves quite calmly). The first MERS-CoV coronavirus epidemic with a 10% mortality rate in Vietnam and China (2002-2003, more than 8000 people fell ill) also stopped quickly. The same thing happened with the MERS coronavirus epidemic in the Middle East (2012-2013, a mortality rate of 33%, about 2,500 people fell ill). There is, for example, human coronavirus OS43. It is assumed that around 1890, a severe pandemic of respiratory infection caused by this virus took place around the world. But now OS43 is one of four peaceful coronaviruses that cause a person to have a cold, which usually follows a benign course.
We can say that the powerful man suppressed diseases with anti-epidemic measures, but as a virologist, I don’t really believe in it. Anti-epidemic measures can reduce and limit the incidence, but not wipe the virus off the face of the earth. Moreover, there were no vaccines at that time, but even if the viruses did not disappear completely, they transformed into a peaceful form and do not cause severe cases. These are the consequences of genetic changes in viruses, and it can be assumed that the same thing will happen with SARS-CoV-2. But no one can accurately predict the timing. I believe that if the whole of humanity undertakes to comply with the necessary measures and vaccinate, then within a year it is possible to transform the virus into a safe form.
– Now there is information that 300 BAU – binding antibody units – are enough to protect against coronavirus infection. This level is constantly decreasing. Is it possible that this immunity will not have to be constantly maintained with vaccines?
– The protective level of antibodies is not a dogma, especially if the antibodies are not detected in the neutralization reaction which uses the variant of the virus that dominates the epidemic today. The level of antibodies is not something permanent.
Antibodies that are produced in response to coronavirus or anti-coronavirus vaccines cannot be constantly at the same level. With immunization, their level will necessarily rise, and, over time, decrease.
But immunity is not only antibodies, so the indicators of 300-500 BAU are conditional. Later this level may decrease, but the immunity will remain. It is believed that it lasts for six months, after which it is worth undergoing revaccination. The need for more frequent revaccination is not ruled out, especially in connection with new variants of coronavirus.
– But is this 300 BAU antibody level guaranteed to protect against Delta or other variants?
– There can be no absolute guarantees. Different variants of the coronavirus can be neutralized by different levels of antibodies directed against a certain variant of the virus. Specialists of The Gamaleya Research Center reported that to neutralize Delta, about 2-4 times more antibodies obtained against the original Wuhan virus are needed. To neutralize the new upcoming Omicron with antibodies to the Wuhan virus, 40 times more antibodies are needed than to neutralize the Wuhan variant itself.
– Are there any studies regarding the genetic predisposition to COVID-19? Are individuals more likely to get sick or be at risk of a severe form of the disease?
– Most likely there is such a phenomenon. There was information about the link between morbidity and different blood types, or rather about certain genetic differences of people with different blood types. It was believed that people with A (II) are most vulnerable to COVID-19 infection, and people with the remaining types are more resistant. There is such a phenomenon, but it is not yet clear how accurate this information is. It is not so easy to identify a group of people resistant to infection.
– Can coronavirus affect human genetics in the future?
– I don’t think that SARS-CoV-2 is one of those viruses that can seriously affect the genetics of humanity due to the selection of survivors. To do this, it must be more pathogenic and cause a higher mortality rate. Of course, this virus can have some impact, but it takes hundreds and hundreds of years of its influence on the human population. Whether it will stay with us for such a period, and how influential it has been in the past and will be in the future is not very clear yet. It is difficult to categorically deny such a possibility, but there is also no reason to agree. Coronaviruses most likely do not have a direct genetic effect on a person by penetrating the genome.
I can say for sure that the vaccines that are currently being used cannot affect human genetics in any way, although this is a fairly common myth. There is a category of people who believe in this. I think it is necessary to fight against such prejudice, conduct a constant awareness campaign, convince people to get vaccinated and revaccinated. This will help overcome the pandemic.
I am a supporter of strict measures regarding vaccination and compliance with anti-epidemic measures. Of course, the pandemic leads to a violation of the rights and freedoms of people who are offered vaccination, makes them uncomfortable (QR-codes, fines). Here they recall the rights and freedoms, forgetting that in a pandemic, the rights and freedoms of one person are too closely linked to the rights and freedoms of another. By refusing the vaccine, not observing anti-epidemic measures, and getting sick, you can infect another person – then what about their rights and freedoms?
The interview was conducted with the support of the Ministry of Science and Higher Education of the Russian Federation and the Russian Academy of Sciences.
Photo: phonlamaiphoto / ru.123rf.com