The human body is unique in every sense. Take, for example, moles – spots on the body that turn our skin into a “map of constellations.” However, not all moles remain harmless. Some of them can be potentially dangerous. Therefore, doctors urge to carefully monitor changes in their shape, color, and size. But if there are many moles, even a professional is unlikely to be able to keep track of each one. The photofixation method, known today as the “skin passport,” allows us to notice the threat in time.
Nikolay Nikolaevich Potekaev – Professor, Chief Dermatovenerologist and Cosmetologist of the Ministry of Health of the Russian Federation, Director of the Moscow Scientific and Practical Center of Dermatovenerology and Cosmetology of the Moscow Department of Health.
– Nikolay Nikolaevich, first of all, tell us what is unique about human skin.
– Human skin is truly unique. Firstly, it is the largest human organ. The area of our skin is about two square meters. Secondly, the skin includes a huge number of protective mechanisms. At the same time, it contains various receptors that are responsible for heat, cold, sensitivity to touch, and also protect us from trouble. For example, touching a hot kettle, we immediately feel a sensation of heat and pull our hands away so as not to get burned.
In addition, the skin provides for thermoregulation. In the cold, our skin becomes paler to preserve energy exchange, and in the heat, it releases a large amount of sweat to cool the body. Therefore, the skin is one of the most important organs, along with the heart, liver, kidneys, and brain.
– Can the skin signal possible diseases in the human body?
– Yes. The skin can indeed give signals about any lesions or diseases of internal organs. For example, lack of oxygen manifests itself in the form of the blueness of the nasolabial triangle, peripheral cyanosis. And this is a typical manifestation of cardiovascular disorders. Simply put, the heart cannot pump blood efficiently through the body, which means the body does not receive oxygen.
With liver damage, the skin turns yellow. And a blush on the face can be a healthy blush after frost or signal a cardiac lesion. If a person suffers from endocrine diseases, the skin becomes pale, flabby.
– Can a person identify certain symptoms by their own skin?
– A person can complain. The symptoms, and how to interpret them, are determined only by a dermatologist.
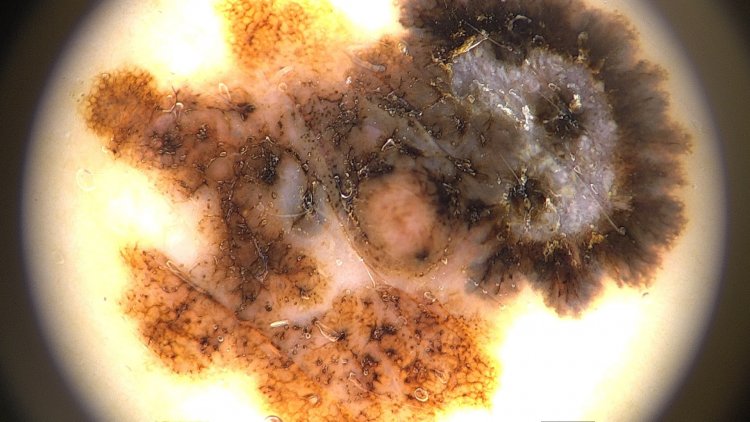
Melanoma of the skin. Dermatoscopic picture. Magnification x20
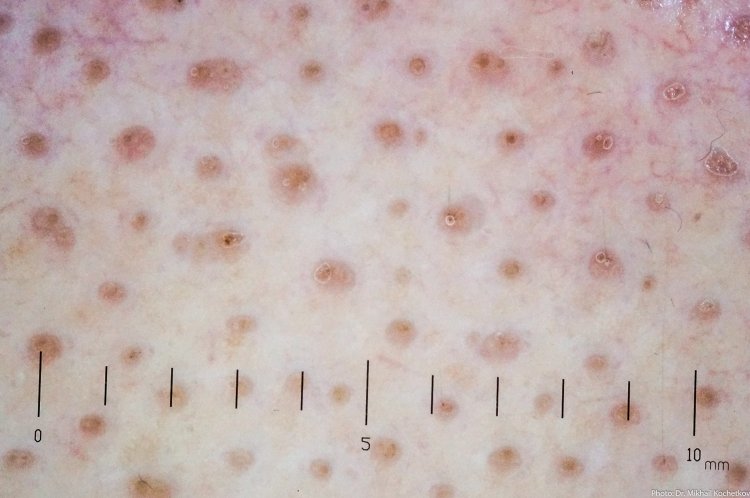
Recurrence of melanocytic nevus in the scar. Dermatoscopic picture. Magnification x20
– When talking about oncological diseases, breast cancer and lung cancer are most often mentioned. What is the place of skin cancer in terms of morbidity?
– Skin cancer, that is, all malignant neoplasms, ranks first in detectability in people over sixty years of age. In addition, in women, skin cancer ranks second after breast cancer, and in men – third after prostate cancer and cancer of the bronchopulmonary system.
– So, this is a fairly common occurrence?
– Yes, indeed.
– What mechanisms of diagnosis and subsequent treatment of skin cancer have been developed to date?
– The basis of diagnosis is the examination of the patient and diagnosis by a dermatovenerologist. To do this, the specialist uses not only the eyes and their own experience but also in some cases auxiliary methods, such as, for example, dermatoscopy. With the help of a dermatoscope, which allows enlarging the image of the skin surface, the doctor can study in more detail the structure and appearance of one or another of its changes. This is especially important if we are talking about neoplasms of the melanocytic type, that is, pigment formation. Because melanoma is the most terrible human tumor along with glioblastoma, a brain tumor.
So, the dermatoscope allows studying moles in detail, which outwardly may seem safe. With the help of this device, the doctor can see the alarming nuances. If a malignant neoplasm is suspected on the skin, the dermatovenerologist directs the patient to an oncologist.
– Continuing the subject of skin diagnostics, I would like to learn more about the skin passport. What is the essence of this method?
– The essence of the method for drawing up a skin passport is the photofixation of all neoplasms, primarily of the melanocytic order. I remind that the skin is two square meters of surface. Therefore, with the help of special equipment, we record all neoplasms in all areas of the patient’s skin. And what is especially important, when drawing up a skin passport, both photographs of the skin and dermatoscopic images of specific areas are used.
Digital dermatoscopy device
Then each element gets its sequence number. And with subsequent studies, we can track the dynamics of changes in certain neoplasms on the skin. First of all, we are talking about nevi or moles.
For example, a person may have a thousand neoplasms. It is clear that on their own, they will not be able to count them, much less notice whether there has been any change with a particular mole, whether it has become darker or more convex, and so on. Even a doctor will find it difficult to diagnose with such an abundance of moles. Therefore, the latest optical equipment, combined with a serious computer program and the capabilities of artificial intelligence, allows us to make the skin passport, which contains information about how many elements, where they are located depending on the serial number and whether any change has occurred with them when the examination is repeated in six months or a year.
– That is, a certain periodicity is important? If a person has many moles, then it is advisable to get checked more often?
– Yes, if a person has many moles, it is advisable to show yourself to a dermatologist at least once a year. At the first visit, the doctor will determine how often you need to come. Because there are many nevi and moles that are always benign in terms of prognosis. But there are also those that remain benign, but from the point of view of prognosis can potentially develop into a tumor.
– And in general, “many” moles are how many?
– In fact, it’s all very individual. In general, from 30 to 50 moles are normal for a person. At the same time, I note that they can be completely different. It may be a simple nevus, or it may be a papillomatous nevus, or an intradermal nevus, which is not even particularly pigmented. But if there are more than a hundred moles, then special attention is required.
Speaking about making a skin passport, it should be noted that this system is very useful in terms of managing the so-called dispensary group of patients, that is, people who have melanoma precursors – moles that can turn, transform into melanoma, for example, the so-called dysplastic nevus. In our Center for Non-Invasive Skin Diagnostics, we keep a register of such patients.
– What types of skin diseases are especially common in our country?
– In general, skin diseases are found all over the world. And there are no differences as such. But, for example, in terms of the melanoma incidence, Russia is about in the middle. At the same time, there are countries in which this disease is quite serious, and many times exceeds the Russian level. And as an example, I would like to cite Australia, where melanoma occurs ten times more often than in Russia.
Candidate of Medical Sciences Kochetkov M.A. in the laboratory of the MSPCDC Center for Noninvasive Skin Diagnostics
The fact is that ethnically and genetically, the population of Australia is represented by immigrants from the northern territories, including the UK, where the climate zone is completely different. At the same time, Australia, as we know, has a hot climate, more sun, so melanomas are more common.
And in general, the sun is one of the main factors that can provoke the development of malignant neoplasms on the skin.
– That is, climatic characteristics also seriously affect the likelihood of such diseases?
– Yes. And since Russia is in the middle climatic zone, the incidence of melanoma is comparable to the level in Central Europe.
But here we are faced with a kind of paradox. It would seem that the incidence of melanoma should be higher where there is more sun. But save for Australia, the incidence of melanoma is higher among people living in the northern territories. Why? The answer is simple. Wanting to make up for the lack of sunlight, people use tanning salons, go to resorts where they try to sunbathe as much as possible. But their skin is completely unprepared for this.
– And what other diseases are of concern to doctors?
– To date, at least two chronic and common diseases are of concern – psoriasis and atopic dermatitis. They are very common in dermatological practice. So, psoriasis affects about 3% of the world’s population, that is, millions of people. This is a very urgent problem since no cure for psoriasis has yet been found. So far, dermatologists have only methods of prolonging remission, that is, the period when there are no psoriatic lesions on the skin, and the patient looks completely healthy. But we must understand that sooner or later relapse is possible, and the disease returns.
As for atopic dermatitis, it is associated with diathesis in children. As a rule, it is diathesis that is considered the first manifestation of atopic dermatitis in the future. Fortunately, atopic dermatitis, unlike psoriasis, is fully curable. And often, starting in childhood, the disease disappears already in the puberty period and after 20. However, atopic dermatitis has another significant and unpleasant aspect – it is often combined with bronchial asthma. This is why in the treatment of patients, dermatologists actively cooperate with allergists-immunologists, as well as with pulmonologists, solving this problem together.
– Let’s talk about the challenges that the COVID-19 pandemic has brought. As far as I know, you are the author of the first classification of skin manifestations associated with the novel coronavirus infection. How was it formed and what is known today?
– Our classification of skin lesions in the novel coronavirus infection was published in August 2020 in the International Journal of Dermatology. What prompted us to create this classification? The reason was the publication of colleagues from other countries. In March 2020, we saw an interesting material – photos of patients with coronavirus infection who had skin lesions. This atlas, let’s call it that, was prepared by Spanish doctors, dermatologists, and therapists. It contained information about 375 observations and changes that were present in patients. These were cases that we also observed in our work. Having collected the material, by summer 2020 we have already proposed our vision and presented seven groups of diseases.
One of the most important and key manifestations is angiitis, or vasculitis, of the skin, that is, vascular inflammatory lesions of the lower and upper extremities. But in the structure of skin lesions in COVID-19, angiitis is not the most common type. But it is this disease that is more often observed in hospitals.
In outpatient settings, with a mild course of coronavirus infection, there are other lesions, for example, “covid toes:” the redness of the tips of the toes. That is, literally an undeveloped form of angiitis. Simply put, if the disease proceeds easily, then only “covid toes” appear. But if we are talking about the severe course of the disease, when there is lung damage, high fever, then skin damage is also progressing. Among other things, urticaria and even Pityriasis rosea are included in the classification.
If we talk about how common skin lesions are in patients with coronavirus infection, then based on the data in the scientific literature and the results that come from medical institutions, I can say that skin lesions occur in about 6% of patients.
– Are there complications from coronavirus infection in the form of skin diseases?
– Yes, I observed quite many patients who came to me after a coronavirus infection with skin lesions. But here I will allow myself to quote a Latin fallacy: “Post hoc ergo propter hoc.” That is, these were patients with angiitis, which occurred two months after the coronavirus infection. Whether this is directly related to COVID-19 is difficult to say.
However, there are consequences of coronavirus infection in the form of post covid alopecia, that is, hair loss. After a person has already recovered, started working, six, seven, or even eight weeks have passed, diffuse hair loss suddenly occurs. Moreover, it is such that people lose up to 40%, and sometimes up to 50% of the hair on their heads. And this, of course, becomes noticeable, delivering tangible internal discomfort, especially in women.
Focal alopecia. Evenly spaced rounded structures at the mouths of hair follicles. Trichoscopic picture. Magnification x20
Postcovid alopecia. The number of telogen (falling out) hair is increased. Trichoscopic picture. Magnification x20
– Is this a reversible process? Or a person may need a hair transplant in the future?
– No, of course, no hair transplant is needed. The specifics of the process are well understood. First, I want to reassure everyone who was a victim of these circumstances, because there are a lot of such people, about 35%. That is, a third of people who have suffered a coronavirus infection suffer from hair loss. We are talking about telogen alopecia. What does it mean? If the hair grows, it means that it is in the anagen phase, if it falls out, it is in the telogen phase. In a normal state, about 80% of our hair is in the anagen phase (growth), and the remaining 20% is in the telogen phase. After a coronavirus infection, this proportion changes.
– Why does it happen?
– There are many different opinions. Discussions are still ongoing. For example, foreign colleagues believe that there is a direct effect of the virus on the hair follicle, which leads to hair loss. Hypotheses are also proposed that inflammatory mediators, cytokines and interleukins, can influence this process.
In our center, we conducted a serious scientific study on this subject. A biopsy of patients who have had a coronavirus infection has shown that in fact, nothing special happens to the hair follicle. We did not find any serious infiltrate that would squeeze the hair follicle, we did not find vasculitis that could disrupt the nutrition of the hair. By and large, the same large amount of hair was observed in the telogen phase, loss, but in general, the skin structure was completely normal.
This suggests that, most likely, hair loss is associated with severe stress experienced by the patient during the disease. The fact is that the hair does not leave its hair follicle immediately, but after some time. Most likely, this is why a noticeable loss is observed not at the time of the disease, but after a few weeks.
– Doctors always remind us of the importance of prevention. If we are talking about skin diseases, what is the prevention in this case?
– Prevention of skin diseases is not much different from general hygienic recommendations. Certain techniques must be followed by persons prone, for example, to dry skin. In this case, they should not overdo water procedures, because water dries the skin, washing away the water-lipid mantle. This is a special film on the skin that protects it from external influences, including bacterial and viral agents. Therefore, the skin needs to be moisturized.
If we are talking about the prevention of aging, then it is worth protecting the skin from sunlight. There is such a term as dermatoheliosis. That is, skin aging under the influence of the sun, or photoaging. Let me remind you that ultraviolet rays not only provoke the appearance of neoplasms on the skin but also negatively affect elastic fibers. Elasticity, that is, the turgor of the skin is one of the important factors that determine its appearance. Smooth elastic skin is a sign of youth. If the skin is flabby and wrinkled, then we are most likely talking about age-related changes. And it is the sun, unfortunately, that contributes to the acceleration of these changes. Therefore, it is worth, at least, using photoprotective means before going out into the sun.
The interview was conducted with the support of the Ministry of Science and Higher Education of the Russian Federation and the Russian Academy of Sciences.