Bipolar affective disorder. It is accompanied by deviations in the biochemical processes of the brain. The word “bipolar” stands for two extremes – mania and depression alternate, while the person is just trying to live.
“Fifteen years ago, I wrote a book about my struggle with mania and depression, about a suicide attempt that nearly became fatal for me, about my stubborn unwillingness to take the medication I needed. It was a hard book, immersing in the hard reality of bipolar disorder. But it was also a tale of the saving power of love, friendship, family, and the gift of a doctor capable of healing,” so begins the afterword by clinical psychologist Kay Jamison for her book on bipolar disorder.
This afterword to An Unquiet Mind reflects both the pain and the hope of people suffering from bipolar affective disorder. There are about 1 to 4 percent of the world’s population affected by this disorder. Of course, it’s impossible to calculate exactly, but even 4% is 320 million people. This is despite the fact that BAD is difficult to diagnose and not everyone goes to a doctor. In fact, the number could be much higher.
The words “depression” and “bipolar disorder” were searched for on Yandex about a million times in March 2021 alone. 700,000 times over the same period in 2020, and 500,000 times in 2019. And although the trend toward taking care of oneself and one’s health, including psychological health, has recently gained momentum, for many people mental disorders are still shrouded in a fog of obscurity, myths, rumors, and stereotypes.
Terminology
BAD is bipolar affective disorder, a pathology accompanied by abnormalities in the biochemical processes of the brain. The disorder is chronic and life expectancy for people with BAD is, on average, 9 years shorter.
The word “bipolar” means – two extremes. The disorder manifests itself in sudden changes in emotions, mood, and energy levels. These changes do not occur instantaneously; they usually last for several days or weeks.
Common characteristics distinguish a depressed state – a depressive episode. It is identical to the condition in a related disorder, unipolar depression. People feel despair, melancholy, lack of energy and mental concentration. This condition can manifest itself physically – in lack or excess of sleeping or eating.
There is also an elevated state, which succeeds the depressive state – a manic episode. This is the difference between bipolar disorder and unipolar depression. In such a state, a person feels energized, happy, and optimistic. Euphoria and high self-esteem are also this stage companions.
In depression, people have suicidal thoughts, they feel guilty and begin to self-injure, they develop certain addictions, such as food addiction, for example. And in mania, people don’t just feel good – they feel literally invulnerable, in every way. They can invest all their savings in a risky business, carelessly engage in dangerous sports. In this stage, the person may reach delusions or manifestations of megalomania – feeling like a messenger from God or having supernatural powers.
Classification
Yes, we all, even healthy people, experience certain stages of “moderate” intensity. In the case of bipolar disorder, the word “too much” is appropriate to describe these episodes. The disorder classification depends on the nature of its manifestation. (Fig. 1)
A person suffering from unipolar depression may have “moderate” rises, but the falls can be crushing and last quite a long time. People with bipolar I disorder experience severe falls that last at least two weeks and then a steep rise that lasts at least a week. If untreated, these manic episodes can last from 3 to 6 months. Bipolar II disorder differs from the first type in that a person does not reach such a high level of instability in the mania stage. This is called hypomania. And it can last for at least four days, but usually such episodes last for weeks or months. In the case of cyclothymia, the falls and rises are less peaky, but they continue alternately for at least two years.
There are also other variations. For example, sometimes a person may experience symptoms characteristic of both phases at the same time. Or these phases may alternate very frequently – 4 or more episodes of depression or mania in a year.
Causes
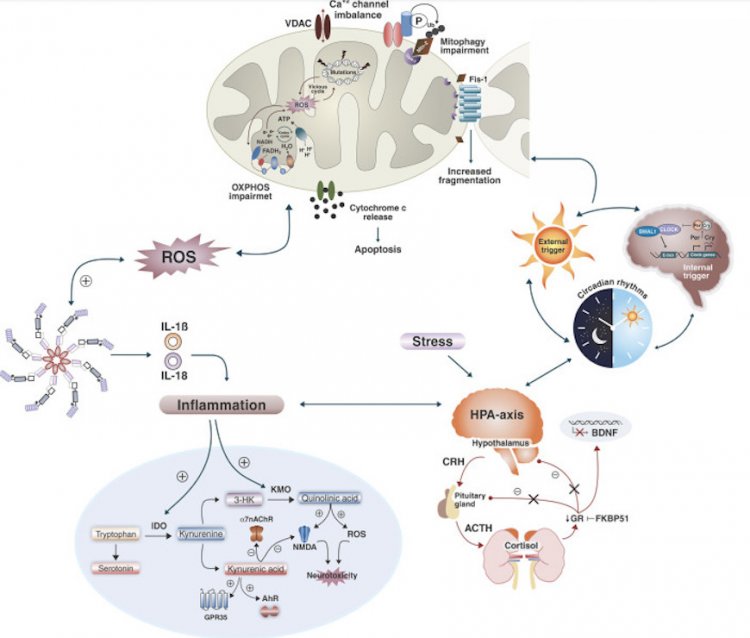
The cause of bipolar disorder is still unknown, as is the case with many other mental illnesses. Nevertheless, scientific research has achieved some results. A dynamic interaction between genetic, neurochemical, and environmental factors has been found to play a role in the onset and progression of BAD. (Figure 2)
Figure 2. Causes of bipolar disorder
It is assumed that the heritability rate is about 70-80%. Scientists attribute such high numbers to two factors: genetic transmission and a “hereditary” family environment, which is potentially disrupted if parents have psychopathology. No “bipolar gene” has been found, but it has been discovered that some interaction between certain genes affects the likelihood of developing the disorder.
A genome-wide association study conducted in 2019 found 30 locations on the chromosome – the loci that contain genes encoding ion channels, neurotransmitter transporters, and synaptic components. Their analysis revealed nine significantly enriched sets of genes that influence the development of BAD. According to the study, the scientists found that bipolar I disorder is strongly genetically correlated with psychosis-determined schizophrenia, while bipolar II disorder is more strongly correlated with major depressive disorder.
Another study of the DNA genome in the postmortem hippocampus in humans found a decrease in the number of copies of mitochondrial DNA (mtDNA) that are located in the mitochondria. Mitochondria are the “energy” stations for all cells of the body – including the brain cells. Scientists believe that preservation of mitochondria and their proper functioning affects life expectancy. Numerous studies over the past 50 years have proven mitochondrial dysfunction in people with BAD and it is considered a pathological factor.
The same study found a strong correlation between the number of mtDNA copies and the length of telomeres, the chromosomes “tips”; their length is closely related to longevity. They also discovered a significant correlation between the acceleration of epigenetic aging and telomere length. Thus, scientists proved an accelerated biological aging of the hippocampus in people with BAD. According to the same scientists, it may account for the neurocognitive dysfunctions of people with bipolar disorder.
Scientists have repeatedly proven that the brain works differently in humans at a certain stage of the disorder.
A healthy brain maintains strong connections between neurons and is constantly renewed. Some unnecessary connections that a person doesn’t use are erased and some new ones are grown. In patients with bipolar disorder the ability to renew is impaired, there are too many connections and the brain is no longer able to navigate around them. And since it cannot navigate, people have abnormal thoughts or behavior.
The BDNF (brain-derived neurotrophic factor), which is involved in all processes of neuronal cell preservation and synapse creation, is considered to be the most studied in bipolar disorder. Such interest in it and several other neutrophins is motivated by the discovery that antidepressants and mood stabilizers can affect these molecules by modulating their signaling pathways.
The amount of BDNF in patients with BAD is low in the brain and blood, and preclinical studies have shown that chronic use of some antidepressants and mood stabilizers, such as lithium and valproic acid, can elevate its levels in the brains of rats. There are studies that confirm the lowered plasma levels of nerve growth factor (NGF) in patients with bipolar disorder. Lithium also increases NGF and GDNF, glial neurotrophic factor, in the hippocampus, frontal cortex, occipital area, and striatum. Neutrophins NGF and GDNF contribute to increased survival, neuronal regeneration, and the emergence of new neuronal connections.
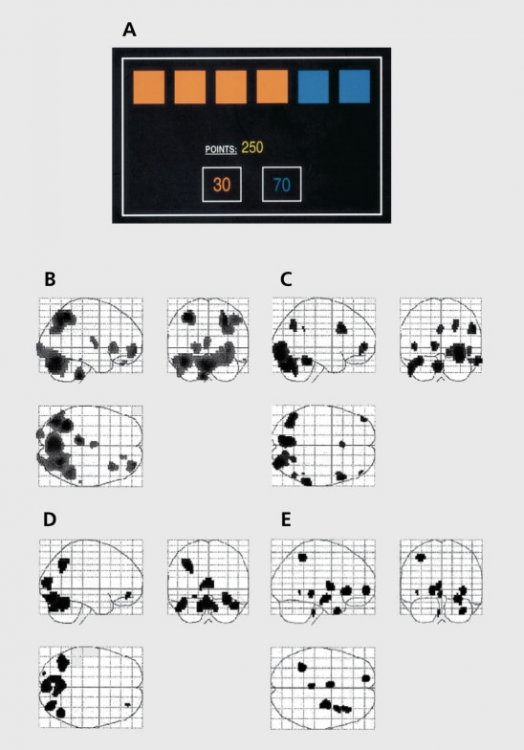
Fig. 3. Brain reactions during risky decision making in manic patients, depressed patients, and healthy individuals.
In 2001, researchers conducted an experiment during which they asked people to solve a neuropsychological task (Fig. 3). People were divided into three groups – mania patients, depressed patients, and healthy people. They monitored the brain’s response to making risky decisions. The subjects were told that there was a certain token hidden under one of six boxes of different colors. The subjects had to guess whether the token was hidden under a red or blue box in order to win points. The less likely option, blue in this example, was also associated with a higher winning value to create a conflict between reward and uncertainty.
Patients with mania had increased activity in the brain area responsible for emotionality, while the area involved in strategic processes and managerial functions was, conversely, depressed. In patients with depression, no significant differences in the activation of brain areas were found.
It is also known that psychosocial stress can also provoke the development of bipolar disorder.
During the clinical treatment of BAD, scientists have discovered abnormalities in the hypothalamic-pituitary-adrenal (HPA) axis, the main mediator of the biological response to stress.
This system releases hormones such as glucocorticoids and epinephrine.Glucocorticoids are steroid hormones that are released by the adrenal glands in response to any stress. Their production is strictly controlled and they affect all three brain neurotransmitter systems – serotonin, noradrenaline, and dopamine, which are considered the “depressive triad.” The production of these hormones affects the synthesis of neurotransmitters, their breakdown, the number of receptors (which turn neurotransmitters into nerve impulses) and their proper functioning.
The brain sends a command in response to stress: to produce some glucocorticoid, which prepares the body to resist the stress, by stimulating the production of neurotransmitters. In order to do this, the hypothalamus uses the corticotropin-releasing hormone in response to stress. It is sent to the pituitary gland to produce adrenocorticotropic hormone, which is further sent to the adrenal glands to increase the production of glucocorticoids. And glucocorticoids, in their turn, stimulate the production of the necessary neurotransmitter. At this stage, as soon as the body senses that a glucocorticoid has entered the bloodstream, the hypothalamus and pituitary gland stop working, the body comes to a standstill and neurotransmitter production ceases.
Abnormalities occur when the negative response of the glucocorticoid cortisol to the hypothalamus and pituitary gland is disrupted, resulting in constant activation of the HPA axis and excessive cortisol release. Disruption of negative response means that cortisol is not stopped from being produced, its receptors become resistant to constant signals, resulting in the increased activity of pro-inflammatory immune mediators and down-regulation of neurotrophic factors such as BDNF. The brain simply does not get the information that cortisol has been produced and does not stop sending “stress pulses.”
This process is also considered one of the theories behind clinical depression. Disruptions in this system lead to impaired sleep patterns, impaired fat burning, disruption of emotions and moods, decreased production of sex hormones, imbalanced neurotransmitters, increased inflammation, and many other consequences. (Fig.4)
Fig. 4.A clear reflection of the set of recent studies on the neurobiological mechanisms of BAD. Biochemical pathways that cause cellular damage.
Summary
There are many studies on the neurobiological mechanisms of BAD, but it is still not
clear what is the primary cause and what is the consequence. Several biochemical processes, not all of which are reflected in the figure above, interact simultaneously to cause cell damage. A vicious circle of multiple systems and mechanisms exacerbate and accelerate cell damage, synaptic dysfunction, and impaired neurogenesis. It leads to progressive structural changes in the brain and cognitive decline, which scientists believe contributes to the neuroprogression of bipolar disorder.
Bipolar affective disorder is not just inability to take control or excessive emotionality. But like depression, it is a mental illness that affects the entire body.
Sources:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6282906/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7524405/#B18
- https://pubmed.ncbi.nlm.nih.gov/31746071/
- https://pubmed.ncbi.nlm.nih.gov/31043756/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181872/
- https://pubmed.ncbi.nlm.nih.gov/11701607/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6489983/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4552246/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1525098/
- https://ironman.ru/news.php?id=5692
- https://www.youtube.com/watch?v=ShsJ6Jr53JI
- https://www.youtube.com/watch?v=RrWBhVlD1H8
Photo on the page and home page: micheile henderson / Unsplash