2021 was announced as Year of Science and Technology, the theme for June being new production technologies and materials. Digital innovations or new materials are developing at lightning speed. Despite our outdated notions, surgeons performing in augmented reality glasses or the use 3D printed dental implants has long stopped being science fiction. The digital era has reached medicine as well.
Starting bio- and 3D-printing
Making human skin, tissue and organs artificially have become a realistic task for modern science. 3D printing and bioprinting mark a new milestone in medical treatment and research.
IT WORKS LIKE THIS
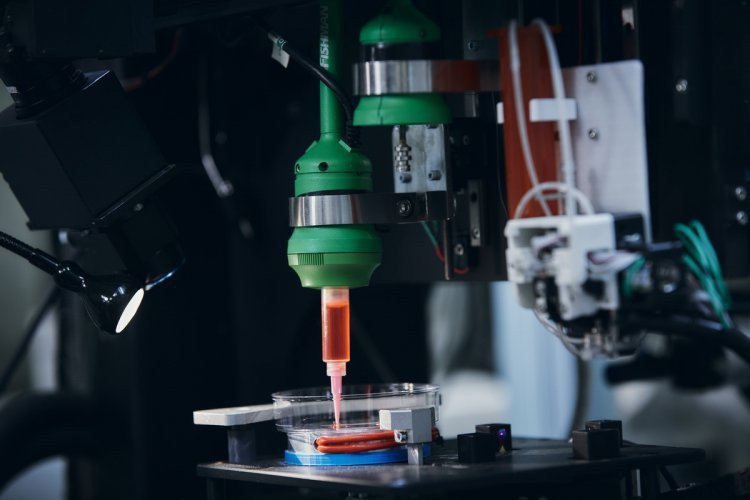
FABIAN bioprinter prints with bio ink
Regular office printers print in two dimensions: the text is created on a flat surface, usually on paper. Measurements used: x (horizontal) and y (vertical).
3D printers add another dimension — depth (z).
During the printing, elements of the printer do not just move up and down, but also left and right, forward and backward. Instead of delivering ink to the paper, the printer distributes special materials — polymers, metal, ceramics, etc. A whole three-dimensional object is created layer by layer, which is called “additive manufacturing”.
But prior to 3D printing, a digital plan has to be made – a 3D model of the object to send to the printer filled with material “prepared” and ready for heating. The printer reads the 3D plan, and its moving parts apply layers of the selected substance one by one. The layers are then transformed into a solid shape using one of several methods: cooling or mixing of two different solutions. Thus several such layers become one element.
Bioprinters work in a similar manner, the key difference being the layers of biomaterial, which may contain live cells. The cells are needed to create complex structures, e.g. blood vessels or skin tissue. Real, living cells are used to do it. They are taken from the patient and cultivated until there is enough of them to make “bio-ink” for the printer.
Printed organs
Now that the printing mechanism is clear, let’s look at application.
Such 3D models are critical for surgical operations. They may help plan the procedure, choose the optimal path for the operation, and take issues that may arise in the process into account.
Mark Berry of Stanford University maintains that it is better to have the chance to plan the operation through and through in advance rather than rely on one’s luck and experience.
3D model printouts can be connected to the “pump” that imitates blood flow. That gives more options to physicians – they can experiment with various paths for endovascular procedures, i.e. treatment of the cardiovascular system without incisions.
The world’s first 3D printed heart was created by a group of scientists of Switzerland's ETH Zurich in 2017. Its prototype weighs only 390 grams. The miniature heart lasts for about 3,000 heartbeats, and was created entirely from human fat cells and human tissue. Unlike its predecessors, this heart was created without the use of synthetic substances. The heart consists of two ventricles, separated by a special chamber serving as the cardiac muscle. An air pump helps the chamber deflate and inflate, allowing the liquid to pump through the heart.
In 2018, bioengineers of the Newcastle University in the United States created a human cornea. The scientists took stem cells from a healthy donor as raw material and added alginate and collagen. The resulting “bio-ink” proved to be optimal for printing. The physicians then used a regular 3D bioprinter at the University to print shapes identical to human corneas within 10 minutes.
Even skeletal bones can be printed out. A team from the Swansea University developed a technology for this. The result was an artificial prosthetic bone made with a biocompatible material that is both durable and regenerative. By the way, it only takes about two hours to print a small bone. Then part of the bone is coated with an adult person’s stem cells that are capable of developing into cells of almost any other type. This is combined with the bio-ink from the printer: polylactic acid (for durability) and alginate (for cell amortization). The product in implanted in the body and disappears completely in about three months, being replaced by a new bone.
Virtual (real)
Augmented reality can be used in medicine for training as well as diagnosis. Special mobile apps are used to “look” into the patient’s body. MITK pille for iPad is designed for surgeons, allowing them to see the patient’s internal organs during surgery.
The visualization becomes possible as a virtual image of the internal organs is superimposed on the real one through the iPad camera.
Another technological solution to help physicians is 3d4medical anatomy platform. It contains numerous quality illustrations and animations. With augmented reality technology, the app builds a 3D model right before the eyes of the user.
Photo on the page and on the main page: Elena Librik/Scientific Russia