At the beginning of the 20th century, Nobel Prize-winning immunologist Paul Ehrlich considered it absurd and impossible that the immune system, meant to protect us from diseases, could attack the body. Today, patients and doctors know that autoimmune diseases are more than real, and some of them are associated with a genetic predisposition. We know around 80 diseases that affect millions of people across the globe. Autoimmune diseases constitute a significant part of endocrine diseases. Why does the immune system attack the body? Why are these diseases more prevalent in women? How does stress cause autoimmune reactions? Ekaterina Anatolyevna Troshina, RAS Corresponding Member, answers these questions.
Ekaterina Anatolyevna Troshina is the Head of the Institute of Clinical Endocrinology at the National Medical Research Center for Endocrinology of the Ministry of Health of the Russian Federation, Doctor of Medical Sciences, and Corresponding Member of the Russian Academy of Sciences.
— When people speak about autoimmune diseases, they mention that the immune system attacks the body. Is it correct to say so?
— Indeed, when we speak about autoimmune diseases, we associate them with friendly fire. It is that sort of a unique situation when immune agents attack the organs of their own body.
Autoimmune diseases constitute a significant part of endocrine diseases. The World Health Organization (WHO) attaches great importance to these diseases. It is no coincidence that WHO declared the 21st century to be “the century of autoimmune diseases.” The share of people suffering from various autoimmune diseases triples every year.
In my practice, I mainly deal with autoimmune endocrine diseases. Though the problems we encounter in our field are, of course, complex and as doctors, scientists and researchers, we must perform a holistic assessment of patients who suffer from autoimmune endocrine disorders.
— Are T cells alone responsible for autoimmune diseases?
— T-cell immunity is the most researched and documented component of the immune system. Scientists and doctors clearly understand the mechanisms of T-cell responses. An equally important component of the immune system, from both scientific and practical perspectives, is B-cell immunity.
We know that regulatory B cells play an important role in the development of autoimmune diseases. Here, it is important to mention central and peripheral tolerance as they are key concepts in immunology. Inadequacies in central or peripheral tolerance lead to autoimmune aggression. Both T-cell and B-cell components are involved in the breakdown of central and peripheral tolerance mechanisms.
When it comes to endocrine diseases, many problems are associated with inadequacies in the major histocompatibility complex (MHC), the so-called human leukocyte antigen (HLA) system. It is an individual set of different types of cell-surface protein molecules. The set of antigens (HLA status) is unique for every person, but certain genetic predispositions lead to the failure of the histocompatibility complex. It is these genetic predispositions that trigger mechanisms, which, in their turn, cause autoimmune diseases.
For example, there are many different disorders of the thyroid gland, an organ that plays an important role in the human body. In fact, this gland regulates all metabolic processes, including fetal brain development.
The painting "The Straw Hat" by the famous Flemish painter Peter Paul Rubens depicts a woman with typical signs of Graves' disease
Healthcare professionals deal with autoimmune thyroiditis and Graves’ disease. These are autoimmune diseases of the thyroid gland accompanied by impairment of thyroid function. One can develop hypothyroidism (underactive thyroid) on the one hand and thyrotoxicosis (overactive thyroid) on the other hand. This is a situation where antibodies kind of replace the thyroid-stimulating hormone receptor. They attach to this receptor and either start stimulating it instead of the thyroid-stimulating hormone or block its function. It causes increased or decreased production of thyroid hormones.
Genetic predisposition does not mean the condition is present at birth; rather, it can be triggered at some point of life, so the disease develops. Most often, these are viral infections or stress responsible for this. Large-scale studies carried out after the Second World War revealed a surge in autoimmune thyroid diseases caused by severe stress. By the way, in women, the trigger might be pregnancy. It does not mean that women should not get pregnant. They should but it is preferable they are aware of the family health history since many genetic factors are inherited, including predisposition to autoimmune diseases.
— Does this mean autoimmune diseases are genetic disorders?
— Right. Patients with an autoimmune disease, typically, autoimmune thyroid disease or type 1 diabetes mellitus, often come to our Institute of Clinical Endocrinology. These conditions are the most common autoimmune disorders in endocrinology. When we examine these patients, we purposefully look for latent forms of other autoimmune diseases.
There are two core types of diseases related to autoimmune polyglandular syndromes. Here we imply a situation where several organs are simultaneously attacked by the body’s immune system. For example, autoimmune polyglandular syndrome type 1 has a clear genetic background. In this case, there is a breakdown in the single autoimmune regulator (AIRE) gene.
Autoimmune polyglandular syndrome type 2 affects the HLA system. Over the course of life, people with this condition successively develop autoimmune thyroid diseases, autoimmune adrenal insufficiency, autoimmune gastritis, and autoimmune diabetes mellitus.
— Following our conversation about type 1 diabetes, I cannot but ask you about its mechanisms. Some research studies suggest that, in people with diabetes mellitus, beta cells produce an increased amount of molecules, which T cells responsible for autoimmune reactions perceive as targets. What is your opinion about this theory? Are similar studies carried out in Russia?
— Of course, such studies are carried out in our country as well. As I have already said, almost all components of the immune system are involved in the development of type 1 diabetes mellitus. Under this scenario, the cells of the islets of Langerhans, the pancreatic beta cells, are affected. Earlier, we believed that type 1 diabetes mellitus developed according to the same laws every time. However, now we are sure that this disease is heterogeneous. Today we see multiple forms of type 1 diabetes mellitus.
— We know that, in most cases, four in five patients are women. Why are autoimmune diseases more prevalent in women than in men?
— It is true. As opposed to men, women get pregnant and give birth to children. As we have already discussed, pregnancy is a strong trigger that can cause autoimmune processes. In addition, there is now an interesting theory of fetal microchimerism. When a child is in the fetal stage, the fetus and the mother share the same blood circulation system. There is a constant interchange of certain substances between them. After birth, substances harboring in the mother's bloodstream are called microchimerism. These residual fetal cells can trigger autoimmune processes in the mother. Indeed, some studies demonstrate that autoimmune diseases are more common in mothers of many children. Again, it does not mean that women should not give birth to many children! Positive protective mechanisms provided by pregnancy to women are undeniable. Women should get pregnant and give birth to children. This process is very good for women's health. However, it is necessary to keep in mind some aspects, especially if there is a certain genetic background.
There are so-called nuclear families when several family members suffer from the same disease. This phenomenon is especially common when it comes to a multifactorial dysfunction of endocrine glands in autoimmune polyglandular syndromes. Therefore, people, today, must know their family health history. It is very important, especially during family planning. Both men and women must be aware of the risks hidden in their genes. If such risks are present, measures should be taken. Today’s technologies allow delivering a healthy child.
Modern science allows for minimizing health risks. Sometimes, it is achieved with the use of preimplantation genetic diagnostics. In this way, future parents can ensure they have a completely healthy child who will not pass on genetic predispositions to future generations.
— Besides stress, what else can trigger an autoimmune reaction?
— We have widely observed these triggers in recent years. Unfortunately, the number of people with autoimmune diseases is increasing amid the coronavirus pandemic. Our center was repurposed as well during the coronavirus peak in Russia. The entire facility was designated as a red zone where COVID-19 patients were treated.
Now we are analyzing our experience and observing people who have been infected. Our results show that the number of people with diabetes mellitus and thyroid diseases is increasing in this group. Some patients suffer from adrenal insufficiency due to the coronavirus infection. We have yet to study how autoimmune endocrinopathies are initiated in connection with cytokine storms that occurred in many patients. Such storms are a protective reaction of the body aimed at destroying harmful agents. However, in their struggle against the virus, cytokines start destroying everything on their way, including healthy cells in certain organs. We face the friendly fire situation again and see the risk of cytokine-induced thyroiditis, adrenalitis, hypophysitis, and so on.
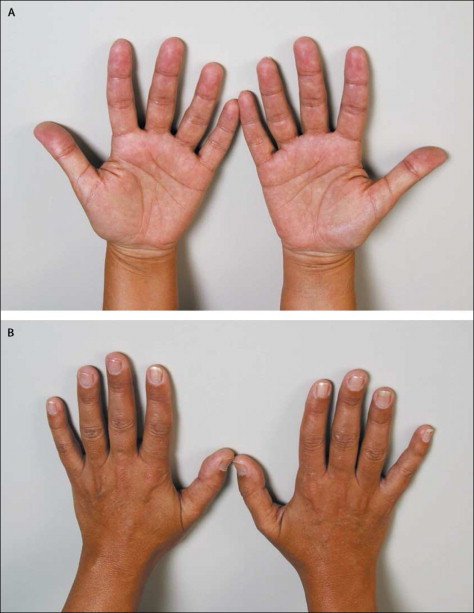
Typical hyperpigmentation of Addison's disease localised to (A) palmar creases and (B) knuckles
— Have you heard of the problem of doctors' distrust of patients who present with unusual symptoms?
— People visit doctors when they are really concerned about something. Therefore, doctors should always treat patients with attention rather than distrust. After all, people visit doctors for a reason, that is, they seek aid and answers to their questions when they feel bad. Even if a patient is unduly alarmed, it still means they have a specific concern, and the doctor’s duty is to help them. Vladimir Bekhterev once said, “If a patient does not feel better after a conversation with the doctor, this is a bad doctor.” The doctor should always assess not only the signs of a specific disease but also a patient’s psychological status. It is essential that patients trust healthcare professionals. Patients’ facial expressions, tone of voice, behavior, and appearance can reveal a lot to a doctor. Changes in patients’ behavior, including emotional lability and excitability, or loginess and apathy, as well as certain skin changes, can be indicative of an autoimmune disease.
For example, a person suddenly develops a local swelling on the back surface of their shank. The swelling resembles an orange peel and does not hurt. In this situation, the person is most likely to turn to a dermatologist. They receive some recommendations but, in many cases, the prescribed treatment does not help. Then, the person starts going around in circles in search of answers. Finally, at some point, they reach an endocrinologist who recognizes the symptoms as the manifestations of a combined autoimmune disease, pretibial myxedema that can accompany Graves’ disease (thyroid disease). One might wonder how the thyroid gland and the shank are interrelated. In the meantime, they are links in the same autoimmune chain. The endocrinologist should immediately understand that this patient is at a high risk of developing another autoimmune disease, that is, endocrine ophthalmopathy or “bulging eyes.” The onset of multiple autoimmune syndrome (MAS) can be triggered by any of the aforementioned factors. As a rule, patients who encounter endocrine ophthalmopathy for the first time would, first and foremost, visit an ophthalmologist and complain about photophobia, excessive tearing, and eye redness. They are treated for conjunctivitis for some time. Topical treatment such as eye drops is prescribed to them, but their eyes soon start to literally stick out of the eye sockets. It hurts them to move their eyes — it is a characteristic symptom of endocrine ophthalmopathy that accompanies Graves’ disease in 50% of cases.
Consider another example: a person suddenly develops persistent weakness. They associate it with vitamin deficiency, stress, fatigue, and sleep deficit. The doctor prescribes vitamins and recommends getting some rest. In the meantime, the patient gets worse and worse. They develop progressive muscle weakness. At some point, along with the weakness, their skin turns darker; they lose weight and develop nausea and salt cravings. All these symptoms are the manifestation of adrenal insufficiency, Addison’s disease. It is a dangerous disease that can lead to death if a person does not receive timely replacement therapy. Primary adrenal insufficiency is of autoimmune nature in 50–70% of cases. Endocrinologists see a lot of unusual and interesting symptoms and, as a rule, those symptoms are associated with autoimmune endocrine diseases.
— Are autoimmune diseases associated with primary immunodeficiencies that may be followed by similar reactions?
— There is such a relationship, in a way, and we keep researching it. There is also evidence that autoimmune diseases of the endocrine organs are more prevalent in people with primary immunodeficiencies.
— You have mentioned a lot of alarming symptoms. How effectively do we cure autoimmune diseases?
— As a rule, any endocrine autoimmune disease leads to either underproduction or overproduction of hormones. Therefore, the main task of an endocrinologist is to either compensate for hormone deficiency or suppress their excessive production. Today, we have well-developed regimens of this therapy and we really help our patients. There is intense research on targeted treatments that totally block the development of autoimmune diseases in people predisposed to them genetically. Our task here is to identify the problem before an autoimmune reaction is triggered. Autoimmune diseases of the endocrine system may be almost asymptomatic at their onset, so people see a doctor only when the clinical picture shows pronounced symptoms that bother a patient. At this stage, the process is already irreversible.
In the meantime, now that we understand how the disease develops and what role genetics play in it, we put our hopes on research on genome editing that will help patients with autoimmune diseases in the future. The National Medical Research Center for Endocrinology is also engaged in such research.
— It is also widely believed that our immune system is insufficiently exposed to natural environments and so it overreacts even to relatively harmless foreign molecules. How true is this statement?
— Reaction is exactly what we need our immune system for. Our immunity is always on guard to defend us. However, sometimes organs that are not supposed to be targeted by antibodies become accessible to their attacks. This is how an autoimmune disease starts.
Ekaterina Anatolyevna Troshina
In and of itself, immunity is the oldest form of biological defense. We encounter microbes and viruses every day. This allows our body to form an immune defense. However, the immune system needs help such as vaccination. We have the National Calendar of Prophylactic Immunization which is systematically revised and extended. Some people say, “I have a weak immune system, so I’m afraid to undergo vaccination.” This is a delusion that turns into dangerous ignorance when one does not trust experts. Conversely, if one’s immune system is really weak, one should undergo vaccination, including coronavirus vaccination. This is the only way to save one’s body from numerous diseases and, in some cases, save your own life and that of your children.
— What is the reason for the rapid increase in autoimmune diseases?
— Our living conditions have drastically changed. People consume larger amounts of processed foods and trans fats and are less physically active. Life has become more comfortable and faster, but we have to pay for this and, in some cases, health is the price.
However, nobody’s canceled healthy lifestyle rules. People are biological creatures, which they have always been. In the meantime, physical activity has been replaced with a sedentary lifestyle. Reduced physical activity, or hypodynamia, leads to a situation where our muscles work less efficiently. In this case, they produce a smaller amount of biologically active substances and hormones that are involved in immune development. The more sitting time one has, the more adipose tissue there is in the body mass. This tissue is a significant producer of many negative pro-inflammatory factors that cause vascular endothelial injury, affect endocrine glands, lead to fatty liver disease, and so on. This blend of biological factors is interrelated with a person’s lifestyle: diet, smoking, and stress. Obese people constitute a huge risk group in terms of autoimmune disease development.
Health is one’s individual responsibility. Of course, the government must create conditions to promote effective healthcare, but it depends on people whether they take advantage of these conditions. For children to be healthy, we need to be a positive role model for them. All healthy habits take roots in a family.
— What about the gut microbiome? It is assumed that it also affects the likelihood of an autoimmune disease.
— Of course! The microbiome is a huge world inside us. It can be our friend or it can turn into an enemy. This relationship between us and the world of bacteria is very old. Therefore, the microbiome is very sensitive to our lifestyle and it changes depending on this lifestyle and, at some point, it begins to affect our life.
Experiments performed at the National Medical Research Center for Endocrinology at the Diabetes Institute focus on type 2 diabetes mellitus, obesity, and microbiome studies. These studies show that when a slim person’s microbiome is transplanted into an overweight patient, the latter begins to lose weight. That is, a slim person’s bacterial colonies can settle in the overweight patient’s intestine and start multiplying there, stimulating specific metabolic processes that lead to a weight loss. This is a very interesting research area in today’s therapy. Now you probably cannot find a health discipline that would not be dealing with human microbiome this way or another.
— Are there any region-specific trends in the spread of autoimmune diseases in Russia?
— Of course, there are. For example, we know that type 1 diabetes is more common in people who live in the northwestern areas of our country. Besides, the overall prevalence of type 1 diabetes increases from the east to the west, from the south to the north. Saint Petersburg, Karelia, and other northern regions of our country are that part of the Russian Federation where type 1 diabetes is most prevalent. This “geography” of type 1 diabetes is recorded in the state diabetes registry that our institution has been maintaining for several decades.
Besides, some endocrine diseases are typical of people living in the south of Russia, mountainous regions, and also in areas where the tradition of consanguine marriages is widespread. I should note that Russia is facing an acute problem of chronic iodine deficiency in its population’s diet, which, in 90% of cases, causes diffuse and nodular goiter, one of the most common endocrine diseases. Unfortunately, Russia still does not legislatively regulate the prevention of iodine deficiency diseases through the mandatory use of iodized salt in a diet. Meanwhile, many other countries have introduced such standards and achieved excellent results. Our country is working on a corresponding law. I am sure that this problem will be solved in Russia, too.
— You have already mentioned that endocrinology is a young science. Meanwhile, there is a shortage of competent endocrinologists in the country. How is this problem solved today?
— In the frame of the national project Healthcare, we have a federal project called “Development of a Network of National Medical Research Centers (NMRCs) and Introduction of Innovative Medical Technologies.” Their purpose is to coordinate and monitor the state of the corresponding medical service. Therefore, the National Research Center for Endocrinology coordinates the Endocrinological Service of Russia. The center’s specialists regularly visit Russian regions to evaluate the progress, discuss problems, and suggest solutions. At the request of the Ministry of Health, the specialists of the National Medical Research Center for Endocrinology prepare relevant analytical reports and develop proposals that are put into practice. Staffing problems are not ignored, of course.
Staff shortage does exist, indeed. However, it is more common in rural rather than urban areas, and it mainly manifests itself in polyclinics rather than in inpatient departments. Hospitals usually have no shortage of endocrinologists, as opposed to polyclinics, to which staff shortage is a problem. It is no secret that the problem is region-specific. Today, local authorities are responsible for independently managing their budgets, including salaries in healthcare. Thus, the distribution of salaries is very asymmetric in a number of regions. There are situations where a region experiences a shortage of doctors, while a neighboring region is overstaffed as it offers more favorable working conditions. This is a pressing issue that has to be addressed.
We must not forget that people have to be trained. Being the leading endocrinology center, we train young doctors. Thus, the National Medical Research Center for Endocrinology annually trains resident doctors from different parts of our country. Besides, our center has an institute of postgraduate and advanced training. Doctors from different regions come to us to undergo training. Then they return to their institutions and share the knowledge they have acquired with their peers.
Of course, staffing is a complex task. A recent graduate with a degree in endocrinology should be eligible for social guarantees in the home region. They must be motivated to stay and work in the region, remain interested in their profession, and help patients using all the knowledge they have acquired in the federal center.
Another important task relates to developing and implementing special federal programs. Today, we have a draft federal program meant to provide systemic care to diabetes mellitus patients throughout our country. This is a matter of national importance. The program will help to attract and train new staff.
We solve all pressing problems in close cooperation with our colleagues from other health disciplines. We work in tandem with general practitioners who are usually the first ones patients turn to – cardiologists, neurologists, immunologists, oncologists, gastroenterologists, gynecologists, rheumatologists, and other specialists. We are in close relationship with all health disciplines today. Endocrinology is everywhere now: no system of the human body can function outside the regulatory activity of hormones.
As to patients, all people want to be healthy. This is the most important thing in life, the basis of harmony. “Harmony is in hormones,” endocrinologists would joke. There’s a grain of truth in every joke! Therefore, if our hormones are okay, we will be healthy.