Since early this year, the reports about COVID-19 have been touching upon the topic of new strains from time to time. Higher incidence rate, heavier progression of disease, possibility of getting infected for the second time, etc. – this is what individual sources write about. To what extent are new trains really dangerous? Can existing vaccines cope with them? What conditions are required to reduce COVID threat to the level of flu? The answers to these questions are in the interview with academic director at the Mechnikov Institute of Vaccines and Serums Vitaly V. Zverev.
Interview with RAS Academician Vitaly Zverev
- South-African, British, Brazilian, Indian – these strains were marked by WHO as alarming on a global level. How many strains are there all in all? Has anybody counted them?
- Each isolated virus is a strain. Each virus isolated in a patient is being studied and compared with the variants isolated in other places: whether they look alike or not.
Viruses are only ones on the planet to contain one nucleic acid – either RNA or DNA. All other organisms contain two types of nucleic acid. DNA contains encoded genetic information, while RNA serves to transform this data into proteins to build this or that organism. As for viruses, they contain either RNA or DNA. The genome of DNA-containing viruses mutates very seldom, unlike RNA-containing ones which are prone to changes.
Coronavirus is not so much prone to mutations, as the virus of influenza or HIV for instance. It mutates by about 30 times slower than the flu virus. As for the strains and mutation, the virus that was discovered in Wuhan and the one that came to Russia from Spain were different: they were divided into the first and second ones. Naturally, the virus continues mutating: we are monitoring the changes to look to what extent these mutations are dangerous.
Mutation means that one nucleotide in genome has replaced another one. It does always lead to the change of protein that codes this gene, yet sometimes even one mutation may result in a drastic change of protein structure.
Let us recall the chronology of coronavirus mutations: first, they talked about South-African one, then English and Brazilian versions appeared, and finally the Indian variant came in. In these cases, the mutations changed the amino acid sequence of spike or S protein, which is expressed on surface: it is responsible for immune development and infective ability of virus. It is this protein that takes part in penetration of virus in sensitive cells of human organism. These mutations look alarming, as it depends upon them whether the virus will become more aggressive.
The first case of infection with English strain happened on December 14. The periodicals immediately reported that this virus spreads much faster and is more hazardous. Now, there are no such messages, they have died out. In fact, the mutation had no impact on the viral spreading rate. It was just that special epidemiological situation favorable for any viral spreading had formed up in the UK at that time. As this very mutation emerged, it was the one to spread.
One of the reasons behind it lay in Brexit (the UK’s exit from the European Union): certain products were not delivered, while people were standing in long lines during bargain sales and therefore forgot about complying with the rules – social distance and masks. Consequently, the virus started spreading much faster. Later, the rush was over, and everything fell into a groove.
- Similar situation was observed in India. Should it be associated with coronavirus?
- There were two main concerns related to mutations. The first one was about the existing vaccines being unable to work due to changes in antigen structure of virus. Second, the specialists feared that the people having gone through the first variant could catch the second one. The Indian strain contained two serious mutations that could influence the structure of virus one way or another.
When the commotion was over and specialists started studying the mutation, it turned out that the serums extracted from the patients having already gone through the first variant could neutralize the new one. It meant that nothing serious had happened, and high spreading rate was related not to mutation, but the conditions in the countries where the new variant has spread. It was the period of religious holiday in India, so crowds of people celebrated it in the streets for several days. The rest are consequences.
In spring last year, abnormally warm weather set in Siberia. TV channels showed people coming out into the streets in Novosibirsk and other regions. The growth in incidence started immediately: people forgot about pandemic and began gathering in large groups, as well as stopped keeping social distance and putting on masks.
Such situations often occur during concerts or meetings. People are gesturing and shouting unaware of being close to other ones. One person at a public event may transmit the infection to thousands of other people.
- Is it related to mutations?
- It is not so far. Naturally, virologists are monitoring the situation.
One cannot say that existing vaccines will be inefficient against new variants of coronavirus. They must protect patients, as they have effect on different parts of protein. There are linear epitopes: the antibodies are generated by a certain amino acid sequence. On the other hand, there are antibodies generated by conformation, as protein does not have linear form, being a complex globule.
Very often, the virus neutralizing antibodies is generated not by these several amino acids, but by the structure, some niche or protuberance on the protein globule. As for existing vaccines, they should work, as no changes that can make them useless have yet occurred. However, it sets off alarm bells, so all changes ought to be monitored.
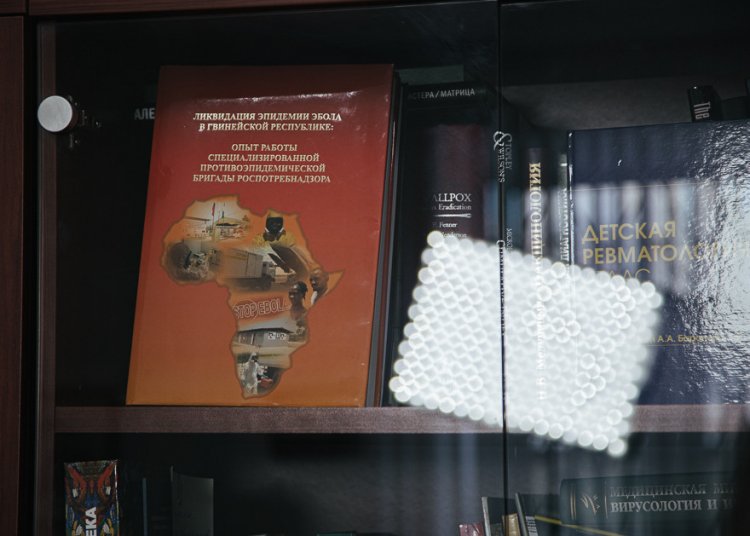
Library in V. Zverev’s office
- Media reported that the re-processing of drugs would take half a year in case a strain that the vaccines cannot cope with appears. Are these reports related to more serious mutations which have not yet come into being?
- More serious mutation should appear, or absolutely new variant of coronavirus, like the one we have now came into being. It has originated from wild nature, from the bats.
Wild nature is the reservoir with a lot of infections, and not only coronavirus ones. So far, the new mutations have impact on the changes in viral structure to some extent, but not to the extent that they start talking about making new vaccines. The situation is under control so far.
- What about the impact of strains on heaviness of disease? Do they cause severer form of illness and raise the fatality rate?
- I have read such publications. To my mind, there is no evidence behind it. So far, there are no grounds to say that the new strain causes heavier infection or raises fatality rate. It is related to different factors as a rule.
Let us take India. Why do we see the highest incidence in the country which outpaces all other ones in the number of vaccinated people? I think that India is a complicated country with serious stratification of society: some people are vaccinated, while others are doomed to fall ill. The same is true for the USA: the incidence affected mostly the poor groups of population consuming unhealthy food and suffering from chronic diseases, obesity above all. The people with high body weight ratio are affected by the virus more than others, as they suffer from diabetes and blood circulation failure.
One disease is added to another one. Please note that the kids either do not fall ill or are mildly sick. The kids that fall ill suffer from some chronic disease as a rule, either a form of cancer or diabetes. Or these are children suffering from obesity. Unfortunately, there are many such children in our country: these may catch a severe form. Young and healthy people account for mild forms as a rule.
– What about the publications saying that strains cause recurrent infection with COVID-19?
- No recurrent case is known for a fact so far. Actually, it may happen, yet due to specifics of human immune systems. It may be single cases so far.
According to official statistics, almost 200 million people have gone through the disease in the world. In fact, this figure is higher: the symptom-free and mild cases, i.e., patients who have not applied to the hospital, are not listed in statistical reports. If there were recurrent cases, media would report about hundreds of thousands or even millions of such cases, not just one or two ones. It would be a problem that everybody could understand and feel. However, it is missing. Thus, we can say that the immunity remains after the patient has gone through the disease. We do not know for how long it remains, but can guess having information about coronavirus.
The immunity for coronavirus variants that have circulated before and failed to cause severe forms can remain for the period of up to one year. Observing the patients having suffered with ARS (atypical pneumonia) we saw that the immunity may remain for up to ten years. The same is true for MERS. The present virus is similar to these ones. I think that those who have gone through the disease may reckon upon the immunity.
- What about the reported recurrent cases then? Was it the undertreated first stage?
- It was either a wrong diagnosis, or chronic form – a single case that may be related to some individual aspect of immune system, the situation when the virus persists in the organism for a long time. We know cases when virus was isolated from a patient for up to 90 days, 3-4 months.
The test systems were unreliable at the initial stage of pandemic, especially the first months. When blood is taken for PCR test, the presence of virus can be detected more accurately. As for nasopharyngeal sample, much depends upon whether it is taken in the right way, and how it I processed and studied afterwards. They say about 100% sensitivity. Yes, it is really a 100% one, yet only in laboratory conditions. When a swab is taken, there are very many factors that can lead to wrong test results.
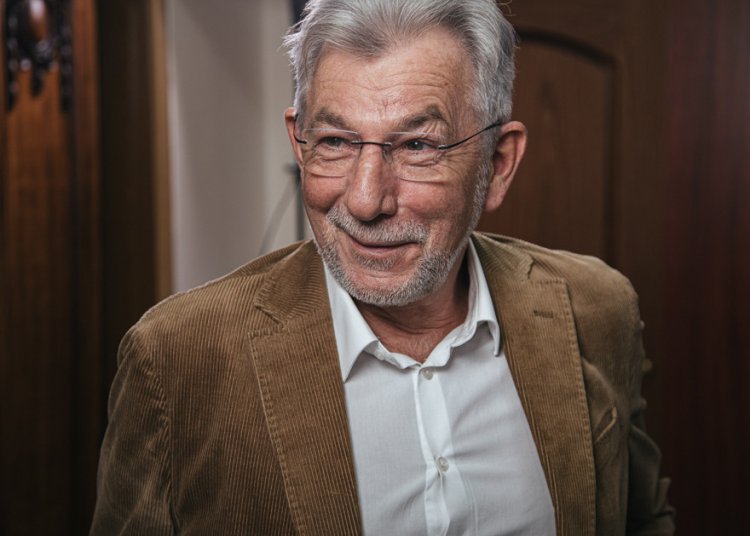
Vitaly Zverev on the territory of Mechnikov Institute
Vitaly Zverev on the territory of Mechnikov Institute
- Can we say that test systems produce result irrespective of coronavirus strain?
- The test systems that we have now work with different parts of genome. The system will certainly identify the virus, but there are very many factors making impact on the test quality.
I know it from my own experience. During the pandemic, I was traveling abroad on business trips a lot and had to undergo medical tests. I have had eight or nine swabs taken, and experience different sensation each time. It depends upon who and how takes them.
– Can we forecast the development of virus, its trains and mutations?
- Unfortunately, it is hard to forecast such things. The mutation is caused by inaccurate work of ferments which replicate viral genome, the so-called RNA polymerases. Some of the ferments work inaccurately as a general matter, like in patients with hepatitis C or HIV.
We talk about quasi-species, i.e., the virus that has got into human organism is different from the one isolated from the patient a year later. We get new specie – the successor of the initial virus modified by mutations. Some mutations lead to the death of virus, others give some preferences to it, enhanced ability to infect for instance. That is why the surviving virus is the one with mutation that let it live further in human population. Virus gains nothing from killing the patient. The patient’s death is a dead-end variant for it. I do not mean that the virus will adjust, stop killing people and tart being transmitted in a non-hazardous way, though it may also happen: everything is possible in virology.
So far, all mutations change the fixation points. For instance, the English variant has higher receptor affinity, yet it has no impact on its spreading rate and severity of illness. Anyway, there is no convincing evidence behind it.
- Yet, physicians knew from the beginning that the virus would mutate, didn’t they?
- Yes, they certainly knew from the very beginning that the virus would mutate like the majority of RNA viruses. There are viruses that mutate slowly, for instance the ones of measles and epidemic parotitis. On the other hand, there are flu and HIV, leaders in mutation speed. Coronavirus mutates by 30 times slower if compared to influenza: about 3 mutations per 30,000 base pairs during the replicative cycle. It is not much.
There may be mutation that will change the properties of coronavirus completely. Now, it is missing and, I hope, will never appear.
– If the coronavirus mutates slowly, can it be eliminated completely?
-We have to learn how to live with it. It has got into human population and will not vanish. Naturally, the present pandemic conditions like lockdown will cease to exist, but a certain percent of people will fall ill every year. New and new people will join the group of potential risk. Those who are young and healthy today will become old and sick tomorrow. That is life!
The virus covered the whole world, all countries. Where will it go to? Over the history of mankind, we have managed to liquidate the virus of natural smallpox alone. We had a reliable vaccine, all countries worked in cooperation, the incidence was lower – individual hotbeds in Africa and Asia – but it took 20 years to cope with it.
- By the way, the smallpox vaccination was involuntary, wasn’t it?
- Yes, sure. As far as I know, in some tribes, tattoos were even used, as they tried to present one and the same person for vaccination several times. It was a complex and serious process, but we should understand that coronavirus is neither smallpox, nor cholera or plague.
I think that new drugs will be produced in the near future, while the physicians will learn to identify the patients belonging to risk groups and start treatment in time. Even now, the mortality rate is not as high as it seems. It is lower than 1%; as official statistics does take into account the asymptomatic patients and kids. It is not by chance that 70% of kids have antibodies in some regions.
- You mean that the virus mutated, mutates and will mutate, don’t you?
- Naturally, it will mutate, while we should monitor the mutations as to the extent of their danger and ability to change the properties of virus. They may result in virus becoming more aggressive and stronger in affecting human organism, as well as immune to vaccines and anti-viral drugs. It may happen, though it is not the case so far, and I hope it will never happen.
- Yet, in this case it will be a different virus, won’t it?
- Sure, it will be. Why do vaccine producers say that half a year is required? It is the time required for transforming laboratory technology into industrial production. A new variant emerges, and the respective vaccine will be produced. They will either modify the existing one or add a new protein, yet time is needed to produce such vaccine in required quantities.
The same has happened today. It took time to enter mass production. Making a vaccine on desktop is one thing, while growing cells in huge fermenters is another thing.
- What is required to transfer coronavirus to the group with the same degree of danger that influenza belongs to?
- It will be done with time. Back in February last year, I said that 70% of people would go through this disease. When it happens, we will come out of pandemic. Everything is heading in that direction today. It is good that we have vaccines. If they are reliable and capable of forming long-lasting immunity, this time will come earlier. If not, the majority of people will still have to go through the disease.
RAS academician, academic director at the Mechnikov Institute of Vaccines and Serums Vitaly Zverev
– Should the recommendations be still complied with?
- It depends upon the recommendations. I believe that we should keep social distance and wear masks, if the distance cannot be kept, like in public places. So far it is mandatory. By the way, it protects not only from coronavirus. Today, we see almost no flu cases, while the incidence of other respiratory diseases has reduced. I.e., these precautions produce certain results.
Nobody has explained to me why gloves are required. To my mind, it is a purely commercial project: somebody wanted to produce and sell them. They protect from nothing. I, a specialist in viruses, also cannot understand why we should wash hands with this rubbish: the virus is not transmitted in such a way. The machines with sanitizers in subway may protect from intestinal diseases in summer, but coronavirus has nothing to do with it.
– So only keeping distance and masks remain the efficient protection measures, right?
- Yes, keeping distance and masks, as well as prophylactic drugs like Interferon and vitamins. However, even vitamins ought to be prescribed by physician. I do not like seeing that people start taking vitamins because they must be taken. Each vitamin is a chemical substance that builds into metabolism. The excess of vitamin is no better than the shortage of it. It is almost the same. Reasonable approach I required.
– Summing up our conversation, there is no point in being afraid of strains today, but the virus is still a threat, right?
- Certainly, it remains a threat irrespective of the strain. They are here and will not go away. You cannot keep the doors locked. The borders are being opened today, so the strains will intermix resulting in new forms. We should keep a wary eye on them, yet they do not lead so far to any crucial change as to prophylactic measures and treatment.
Interview with RAS Academician Vitaly Zverev
Interview was taken with the support of the Ministry of Science and Higher Education, as well as the Russian Academy of Sciences.