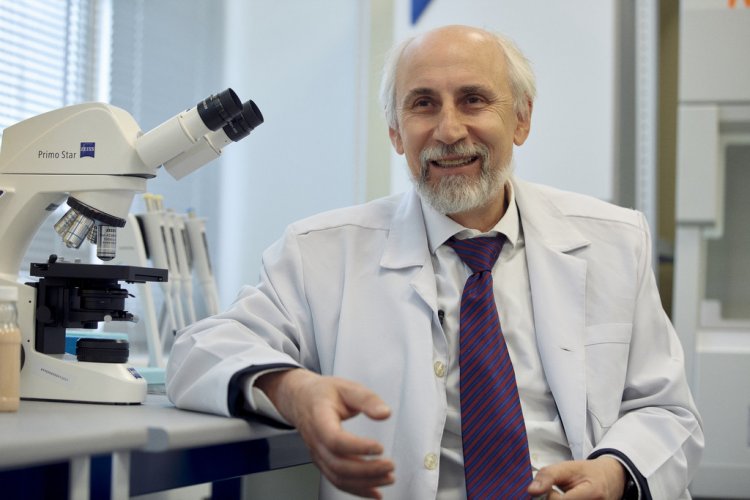
Earlier this year we learned about the creation of an unusual edible vaccine based on probiotics. The idea belongs to a team of scientists from the very first Institute of Experimental Medicine in St. Petersburg, which was the home of the world's first polio vaccine and a live attenuated influenza vaccine. At the beginning of the 20th century, the IEM scientists created drugs to treat plague patients. The archives of the IEM museum contain preserved historical documents describing the history of creation of the “The IEM Special Laboratory for Production of Anti-Plague Medications .” It became known as the “Plague Fort” (Fort Alexander I, located on an artificial island in the Gulf of Finland). Twenty epidemiologists risked their own lives to create an anti-plague vaccine there. No wonder that with the arrival of a new coronavirus infection, the IEM scientists immediately joined the fight for the health of the Russian people. When can we expect a new edible vaccine? And what advantages will it have? Alexander Suvorov, Corresponding Member of the Russian Academy of Sciences and Head of the Department of Molecular Microbiology and the Laboratory of Molecular Genetics of Pathogenic Microorganisms of the IEM, the author of the idea, answers these questions.
Aleksandr Nikolaevich Suvorov is the head of the Department of Molecular Microbiology and the Laboratory of Molecular Genetics of Pathogenic Microorganisms of the IEM, a Corresponding Member of the Russian Academy of Sciences.
– Aleksandr Nikolaevich, tell us about the unique development of an edible vaccine. How did you come up with this idea? How far did the research go?
– The idea to create a mucosal vaccine against coronavirus came immediately after the outbreak of the epidemic was reported. For some reason, many people accused the Chinese of hiding the fact that the epidemic had begun. However, in the meantime, the information about the nucleotide sequence of the new viral pathogen appeared in the databases rather quickly. At that point, we realized that the developments involving the use of probiotics as a platform for creating a vaccine, which had previously been conducted at the Institute of Experimental Medicine, could also be applied to combat SARS-CoV-2.
Historically, our Department of Molecular Microbiology, which was founded by Artem Akopovich Totolyan, Academician of the Russian Academy of Sciences, has long focused on various gram-positive microorganisms, particularly streptococci. Later, when the sphere of our interests expanded, it became clear that it was very important to understand not only the specifics of pathogenic microorganisms, which we have always specialized in, but also that of useful microorganisms. In the early 2000s, we studied a number of bacterial strains of probiotics related to sour-milk bacteria, as well as the genome of beneficial bacteria. We isolated a bacterial strain that was traditionally used back in the Soviet Union as a probiotic in prophylactic products with vitamin properties – Enterococcus faecium L3. It turned out that this strain has a number of unique, beneficial properties for people. We were particularly surprised by its ability to kill harmful bacteria and viruses.
It took us a long time to double-check our results, to see if it actually had antiviral activity. The data were confirmed, as was the ability of the strain to affect the human immune system.
By 2010, once the data of full-genome sequencing of the bacterial strain was available, we came up with the idea of using it as a starting bacterial strain for vaccine development. It must be said that the ideology of making new vaccine drugs is currently undergoing dramatic changes. At a certain point of development, humanity calmed down. We developed a vaccination calendar, all sorts of antibiotics appeared in our arsenal. It seemed that we could easily resist any infectious pathology with this set. Meanwhile, the 21st century hit everyone with a sharp increase in cardiovascular diseases and cancer, as well as the growth of immunopathological and metabolic diseases. The human race began to gain weight unexpectedly quickly. And type 2 diabetes is now starting to affect huge segments of the population. It is all part of the so-called metabolic syndrome. And it is unclear what should we do about it. Because it's not possible to solve these problems and some new challenges with drugs.
And the widespread use of antibiotics has led to the fact that we have created a “monster” – a huge number of bacterial strains carrying what is known as multidrug resistance. Multidrug-resistant bacterial strains have become so “armed to the teeth” that there is no way to fight against them. The “remove and kill the pathogen” principle no longer works.
Therefore, we started looking for new approaches to restore the microbiota and suggested using probiotics to combat harmful bacteria. And when the infectious threat reappeared, we decided to use probiotics as a platform for creating antiviral and antibacterial drugs. We managed to modify a bacterial strain by introducing pathogenic bacterial genes into its genome. Thus, we created several variants of a probiotic that exhibits the genes of pathogenic streptococci and pneumococci. The experiments on laboratory animals showed that mucosal vaccines are effective. In our case, we get a kind of probiotic product with a taste of ryazhenka (fermented baked milk) or kefir, which protects against a particular pathogen beyond the concept of drug resistance.
From the History of the Institute of Experimental Medicine: Plague Fort. Work in the “red zone,” searching for the best vaccine donor. Infecting a camel with plague pathogen
This is an absolutely new approach, based on the creation of targeted vaccines that target not a specific pathogenic species, but a specific strain that causes the disease. This is especially relevant because of the recent evidence that a patient's own microorganisms can cause severe infectious diseases. Each of us has a different microbiota. And what works for some people, may not work for others. The same is true for the body's reaction to dealing with a new coronavirus infection. Using the mucosal vaccine, we train the immune system to fight a specific pathogen.
– What was the basis for the earlier development?
– The first viral target was the influenza virus. We inserted different sections of the influenza virus in order for the immune system to respond against specific viral proteins. A number of so-called “vaccine candidates” against different strains of influenza virus with different serological features were created. The advantage of this kind of probiotic product is that once we create a bacterial strain, we can scale it up quickly. Simply put, we can start production at any dairy plant.
In the case of the drug against coronavirus, our bacterial strain was transformed into a food-based fermented milk product. But it can also be created in the form of capsules, sprays, or pastilles.
I think that this approach of creating food vaccines with the use of probiotics can be considered very promising, because it is simple, transparent and safe.
When we consume the drug with food, we train the organism immediately and protect it from infection. In the case of coronavirus, this is especially valuable because the gastrointestinal tract is considered to be the main route of the pathogen transmission.
– How far is this drug from being finished?
– Today, we still continue to design the drug for further clinical trials. Since the virus is changing very rapidly, we are creating several different variants at once, analyzing the production of a specific immune response. Now we conduct tests on laboratory animals – mice – to check the adaptive immune response, i.e., the production of antibodies and the cellular immune response.
– Does the government have any interest in your development?
– The support is mainly related to the funding of the world-class Scientific Center. But that is not enough to conduct full-scale clinical trials. Since, it is not possible to work with a real virus in all places, unfortunately, now we are looking for commercial partners who could allocate funds for experiments on protectivity.